OFFPRINT
Evolution in time and scales of the stability of
heart interbeat rate
R. Hern´
andez-P´
erez, L. Guzm´
an-Vargas, I. Reyes-Ram´ırez
and
F. Angulo-Brown
EPL,
92
(2010) 68006
T
ARGET YOUR RESEARCH
WITH
EPL
Sign up to receive the free EPL table of
contents alert.
December 2010
EPL,92(2010) 68006 www.epljournal.org
doi:10.1209/0295-5075/92/68006
Evolution in time and scales of the stability of heart interbeat rate
R. Hern´andez-P´erez1(a), L. Guzm´an-Vargas2, I. Reyes-Ram´ırez2,3 and F. Angulo-Brown3 1SATMEX - Av. de las Telecomunicaciones S/N CONTEL Edif. SGA-II, M´exico, D.F. 09310, M´exico
2Unidad Profesional Interdisciplinaria en Ingenier´ıa y Tecnolog´ıas Avanzadas, Instituto Polit´ecnico Nacional
Av. IPN No. 2580, Col. Ticom´an, M´exico D.F. 07340, M´exico
3Departamento de F´ısica, Escuela Superior de F´ısica y Matem´aticas, Instituto Polit´ecnico Nacional
Edif. No. 9, U.P. Zacatenco, M´exico D.F., 07738, M´exico
received 14 August 2010; accepted in final form 7 December 2010 published online 19 January 2011
PACS 87.19.Hh– Cardiac dynamics
PACS 89.20.-a– Interdisciplinary applications of physics
PACS 89.75.Da– Systems obeying scaling laws
Abstract– We approach heart interbeat rate by observing the evolution of its stability on scales
and time, using tools for the analysis of frequency standards. In particular, we employ the dynamic Allan variance, which is used to characterize the time-varying stability of an atomic clock, to analyze heart interbeat time series for normal subjects and patients with congestive heart failure (CHF). Our stability analysis shows that healthy dynamics is characterized by at least two stability regions along different scales. In contrast, diseased patients exhibit at least three different stability regions; over short scales the fluctuations resembled white-noise behavior whereas for large scales a drift is observed. The inflection points delimiting the first two stability regions for both groups are located around the same scales. Moreover, we find that CHF patients show lower variation of the stability in time than healthy subjects.
Copyright cEPLA, 2010
Introduction. – Analysis of heart rate variability using nonlinear tools have shown that the heart rate is related to different frequency components derived from a large number of control mechanisms from the autonomous nervous system [1]. Recent evidence of studies of heart rate variability indicates that healthy systems even at rest display highly irregular dynamics with multifractal character [2], and subjects with congestive heart failure (CHF) exhibit changes in this multifractality with time [2]. Moreover, different studies conducted on heart interbeat have revealed quantitative differences in the fractal organization and correlation properties between healthy and diseased subjects, by using different tools from statis-tical physics and nonlinear dynamics [2,3]. Among the methods that have been used for the analysis of heartbeat signals are: detrended fluctuations analysis [4,5], power spectral density [6], fractal dimension [7,8], multi-fractality [2,9], Allan and Fano factors [6,10], wavelets [1,11] and excursions [12].
In this work, we are interested in studying the stability of the heartbeat interval rate by using the Allan variance statistics. The Allan variance was introduced in the
(a)E-mail:ricardohdzpz@gmail.com
field of time and frequency metrology to quantitatively characterize the frequency fluctuations observed in precise frequency standards, which exhibit nonstationarities that are not satisfactorily treated with conventional statistical tools, such as the classical standard deviation [13]; and it has become a standard to define quantitatively the frequency instabilities of an oscillator; that consist of any unwanted departure from its nominal frequency valueν0; i.e., frequency stability is the degree to which an oscilla-tor produces a constant frequency over a specified time interval [14]. Recently, the dynamic Allan variance was developed, which is a representation of the time-varying stability of an atomic clock and it has been reported its effectiveness in tracking common nonstationary features of an oscillator [15]. Previous studies in the statistical features of heartbeat dynamics, such as using the Allan factor to count the number of beats in different time windows [6] or those using the segmentation method [16] or excursions [12], analyze the statistics and scale invariance of the heart interbeat signals for multiple scales. In the present work we map the heart beat to the “tick” of a precise oscillator (which is subject to noise) to take advantage of statistical and conceptual tools developed in time and frequency metrology for the
R. Hern´andez-P´erezet al.
quantitative characterization of frequency instabilities in an oscillator. Therefore, we study the stability of the heart interbeat interval rate, applying the dynamic Allan variance to: i) identify nonstationarities in the heart interbeat time series; ii) quantify the evolution of stability with scales and time; and, iii) assess how these properties change for healthy and diseased subjects.
Our stability analysis shows that healthy dynamics is characterized by at least two stability regions along different scales. In contrast, diseased patients exhibit at least three different stability regions; over short scales the fluctuations resembled white-noise behavior whereas for large scales a drift is observed. The inflection points delimiting the first two stability regions for both groups are located around the same scales. Interestingly, we find that CHF patients show lower variation in time of the stability than healthy subjects.
Methods. –
Allan variance. In time and frequency metrology, the normalized frequency deviationy(t) of the oscillators (most commonly atomic clocks) is defined in terms of the nominal oscillator frequency ν0 and the instantaneous frequency ν(t) as: y(t) = (ν(t)−ν0)/ν0 [13]. The Allan variance (AVAR) is used as a standard to define quantita-tively the stability of an oscillator. The definition of AVAR is given by the expression σ2
y(τ) =12(¯yt+τ−y¯t) 2 [13],
where τ is the observation interval, the operator · denotes time averaging and the average frequency devi-ation ¯yt is defined as ¯yt=τ1
t+τ
t y(t′) dt′. In discrete
time, the AVAR is computed from frequency deviation data with the following estimator: ˆσ2
y[k] =
1 2(M−2k+1)
M−2k+1
j=1 (¯yk[i+k]−y¯k[i])2 [13], where M
is the total number of data points, τ0 is the minimum observation time interval, and the integer k=τ /τ0 represents the discrete-time observation interval typically taking valuesk= 1, 2, . . . ,⌊N/3⌋(see footnote 1) (where ⌊·⌋ denotes integer part), and the averaged frequency values are given by ¯yk[i]≡k1ji+=ki−1y[j]. The AVAR at
a particular scale is directly related to the variance of wavelet coefficients at that scale when Haar wavelet filters are used [17].
The frequency deviations of frequency standards are either systematic or stochastic. The latter are often well described by power-law spectral processes:Sy(f)∼fβ; for
which AVAR has an interesting property: it exhibits a power-law behavior:σ2
y(τ)∼τη, where the exponents are
related byη=−β−1 for−2β0 [13]. Another way to write the scaling relation is through the Allan deviation:
σy(τ)∼τη/2∼τµ, (1)
1It is a convention extensively used in the time and frequency
metrology field, and it is related to the uncertainty in the estimation of the Allan variance, which for a given averaging time is propor-tional to the number of differences that contribute to it.
200 400 600 800 1000 −5
0 5
t y(t)
100 102 104 10−2
10−1 100
τ σy(τ)
0 200 400
600 800 1000 100
101 100
t τ
σy(t,τ)
−0⊲5 (a)
(c)
(b)
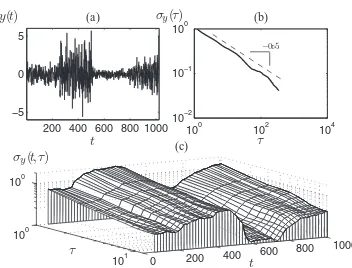
Fig. 1: (a) Synthetic nonstationary time series representing the frequency deviation of an oscillator (N= 1024); (b) its AVAR, σy(τ) vs. τ (stability plot); and, (c) its DAVAR (Nw=N/8). According to AVAR, the signal seems a white noise (µ=−0.5);
while, DAVAR captures the nonstationarities and the changes in the variability of the signal.
with−0.5µ0.5, whereµ=−0.5 corresponds to white noise,µ= 0 to 1/fnoise andµ= 0.5 to Brownian motion2. This scaling property allows the identification of certain stochastic components in a signal (fig. 1).
Dynamic Allan variance. The dynamic Allan vari-ance (DAVAR) was recently developed for the study of nonstationarities in atomic clocks [15]. It is obtained by calculating the estimator ˆσ2
y[k] of AVAR for the
data contained in a window of certain length that slides through the data. Thus, DAVAR provides a way to quan-tify the evolution in time of the stability. The DAVAR is a deterministic quantity defined as the expected value of the estimator [15]: ˆσ2
y[n, k] =2(Nw−12k+1)
n+Nw/2−2k
m=n−Nw/2(¯yk[m+ k]−y¯k[m])2, n=t/τ0 is the discrete time, Nw is
the length of the analysis window3, the averaged frequency values are computed with ¯yk[i]≡k1ji+=ki−1y[j],
k= 1,2, . . . ,⌊Nw/3⌋and the sum runs fromm=n−Nw/2
tom=n+Nw/2−2k−1. The DAVAR is represented by
a 3-D graph showing the variation of the oscillator’s stability (fig. 1(c)). Thus, DAVAR at timet can be inter-preted as a representation of the instantaneous stability of the oscillator; which is the result of an averaging process on the analysis window of length Nw [15]. Since
noisy signals with power-law spectra follow a scaling law in the AVAR (eq. (1)), understanding whether there are nonstationarities in the clock behavior depends on identifying the changes in the scaling exponentµ.
Heart rate dynamics. – There is a debate about whether it is preferable to analyze heartbeat with reference to real time or to beat number. In ref. [10], two methods
2According to the relation between the spectral (β) and Hurst
(H) exponents [6], the following relations hold:µ=H−1 for−1< β0 andµ=H, for−2β−1.
3Selecting the window lengthN
w is a trade-off of two opposite
[image:4.595.335.511.82.216.2]Evolution in time and scales of the stability of heart interbeat rate
are adapted for analyzing the data from each perspective. The first approach treats the heartbeat as the event of interest and assumes that there is an objective “clock” for the timing of the event and that a heartbeat time record can be treated as apoint process,i.e., a sequence of events (beats) distributed on the time axis. This approach was followed in ref. [6], using AVAR to quantify changes in heartbeat time series for heart-failure and normal patients. The second approach emphasizes the interbeat interval and uses the beat number as an index of the biological time.
In the identification of the heartbeat with the frequency deviations of an atomic clock, we use an intermediate approach: what we consider as the input signal is the duration of the interbeat interval (time between two consecutive beats). This signal is indexed with the interval number, on which the definition of the “scales” τ in the AVAR is based. Thus, the stability is referred to the variation in the duration of the interbeat interval for different “scales”. Then, instead of talking about the stability in a certain time scale, we talk about the stability at a certain interbeat scale (certain number of interbeat intervals). The advantage of this approach is that it allows studying the evolution of the important quantity: the interbeat rate, i.e., the frequency of the oscillator (the heart in this case).
Stability of heart oscillations. The concept of home-ostasis, that refers to the tendency of biological systems to maintain a relative constancy of the internal environment (blood sugar, blood pressure and the like) after perturba-tion [18], led to the proposal that physiological variables, such as the cardiac interbeat interval T(n), maintain an approximately constant value in spite of continual pertur-bations. Thus one can write in general T(n) =T0+ξ, where T0 is the preferred level for the interbeat interval and ξ is a white noise with standard deviation σ [18]. Therefore, homeostasis is strongly related to the stability of the heart interbeat intervale rate. Since the heart can be thought of as an oscillator, the applicability of AVAR seems very natural. Therefore, mapping the heart inter-beat to a frequency standard is relevant, and then, apply-ing DAVAR to the heart interbeat time series for healthy and unhealthy subjects would draw some conclusions on the stability of the heart signals; for instance, it allows studying the evolution of the stability of the interbeat rate for both groups.
Evaluating changes in the stability of interbeat interval rate. We are interested in quantifying the evolution of stability in scales and time of the heart interbeat rate. For this task we introduce two parameters, namelyµt(τ)
and γτ(t), which are computed from the DAVAR, and
represent the change of DAVAR with respect to scale and time, respectively.
The parameterµt(τ) quantifies the local slope, at timet
fixed, of DAVAR with respect to the scaleτ,i.e., changes in the slope of DAVAR (in the plane logσy(t, τ)vs.logτ)
0.5 1 1.5 2 2.5 3 x 104
0.4 0.6 0.8 1 1.2 1.4
RR interval (a)
0.5 1 1.5 2 2.5 3 x 104
0.4 0.6 0.8 1 1.2 1.4
[image:5.595.315.535.84.170.2]RR interval (b)
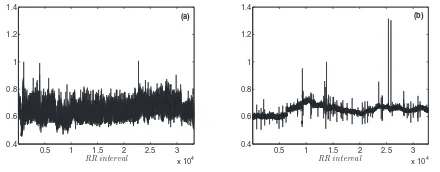
Fig. 2: Diurnal records of (a) a normal subject and (b) a CHF patient.
over scales for a fixed time window; and it is defined as
µt(τ)≡
∂logσy(t, τ)
∂logτ
t
, (2)
which can be estimated by
ˆ
µt(τ) =
Δ log ˆσy(t, τ)
Δ logτ . (3)
Notice thatµt(τ) represents the instantaneous exponent
of the scaling law in the Allan deviation (eq. (1)). This parameter is similar to the one used in ref. [10] to estimate the deviation from power-law scaling by applying the Allan factor to the counts of the number of beats.
On the other hand, the parameterγτ(t) quantifies the
local slope, at scaleτfixed, of DAVAR with respect to time
t, i.e., changes in DAVAR over time (different analysis windows) for a fixed scale. It is defined as
γτ(t)≡
∂σy(t, τ)
∂t
τ
, (4)
which is estimated by
ˆ
γτ(t) =
Δˆσy(t, τ)
Δt . (5)
Both parametersµt(τ) and γτ(t) will produce a
three-dimensional surface, representing the variation of the heart interbeat rate stability in scale and in time, respectively.
Results. – We analyze RR interval sequences from two groups: 16 healthy subjects and 12 CHF patients [19], with 6 hours of diurnal ECG records each with length
N∼30000 beats (fig. 2). Notice that the normal subject exhibits a higher variability than the CHF patient, although the latter exhibits more spikes and jumps than for the normal subject. This database is an extended set of records which we have used in previous studies [9,12]. We compute DAVAR for each time series, considering windows with Nw=⌊N/30⌋ ∼1000 points, with steps of
size⌊Nw/4⌋ ∼250 points and for scalesk= 1,2, . . . , kmax,
with kmax=⌊Nw/3⌋ ∼333 points. This selection, after
computing other options, allows having enough data points to have good confidence in the estimation of AVAR and tracking quick variations in the signals [15].
The stability analysis plots illustrating the results of DAVAR for records of a normal subject and a CHF patient
R. Hern´andez-P´erezet al.
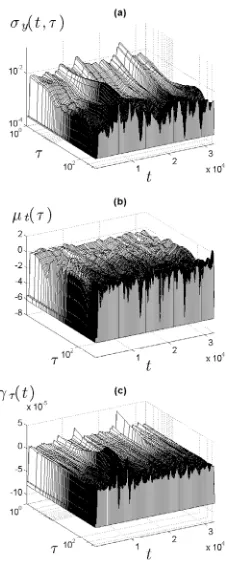
Fig. 3: Stability analysis for a normal subject (fig. 2(a)): (a) the DAVAR profile; (b)µt(τ), where each line corresponds to an analysis window (time fixed); and, (c)γτ(t), where each line corresponds to one scale.
are shown in figs. 3 and 4, respectively. The DAVAR profile for the normal subject (fig. 3(a)) shows a less changing behavior than for the CHF patient (fig. 4(a)), suggesting that for the latter there are more nonstationary features in the signals. The more changing behavior for the CHF patient is captured by µt(τ) (fig. 4(b)). Moreover, γτ(t)
provides the evolution in time of the value of DAVAR for a given scaleτ, and for the CHF patient it is observed a smoother surface (fig. 4(c)) than for the normal subject (fig. 3(c)), although with some noticeable peaks.
Since both parametersµt(τ) andγτ(t) provide a surface,
thus, to summarize the results for each group, we averaged them over time, denoted by·t, and over scales, denoted
by ·τ; such that averaging over time(scales) gives the
mean value of the parameter for a certain scale(time). Figures 5(a) and (b) show the average values for µt(τ)
for records of normal and CHF subjects, respectively, with time averages shown in the main plots, and scale averages in the insets. The behaviour of the averages for each group of subjects is remarkably different. For normal subjects, two inflection points are observed for the average scaling exponent µ over the scales (resulting in three regions), while for the CHF patients there are three inflection points (leading to four regions). The first two inflection points for each group occur approximately at the same scales: ∼10 and ∼60 interbeat intervals, respectively, while the third inflection point for the CHF group occurs at∼120 interbeat intervals. Inflection points
Fig. 4: Stability analysis for a CHF patient (fig. 2(b)): (a) the DAVAR profile; (b)µt(τ); and, (c)γτ(t).
0 50 100 150 200
−0.8 −0.4 0 0.4
τ ¯
μt
0 1 2 3
x 104
−0.5 0 0.5
t ¯ μτ
(a)
0 50 100 150 200
−0.8 −0.4 0 0.4
τ ¯
μt
0 1 2 3
x 104
−0.5 0 0.5
t ¯ μτ
(b)
0 50 100 150 200 −5
−4 −3 −2 −1 0 1 2x 10
−6
τ
¯
γt
0 1 2 3
x 104 −1
0 1x 10
−4
t
¯
γτ
(c)
0 50 100 150 200 −5
−4 −3 −2 −1 0 1 2x 10
−6
τ
¯
γt
0 1 2 3
x 104 −1
0 1x 10
−4
t
¯
γτ
(d)
Fig. 5: (Colour on-line) Average values of parametersµt(τ) and
γτ(t) for normal ((a), (c)) and CHF ((b), (d)) subjects. Time average is shown in the main plots, and scale average in the insets.
at ∼60 beats is consistent with previous studies [20]. Moreover, scale averages for normal subjects are negative, while for CHF subjects they fluctuate around zero. The time average values for ¯µt(τ) for the CHF patients have
[image:6.595.110.215.88.355.2] [image:6.595.315.531.415.578.2]Evolution in time and scales of the stability of heart interbeat rate
−1 0 1
−1 0 1 µ τS (a) µ τ L µ τ L
−1 0 1
−1 0 1 µ τ S (b)
−1 0 1
−1 0 1 µt S µ t L (c) µ t L
−1 0 1
−1 0 1 µt S (d)
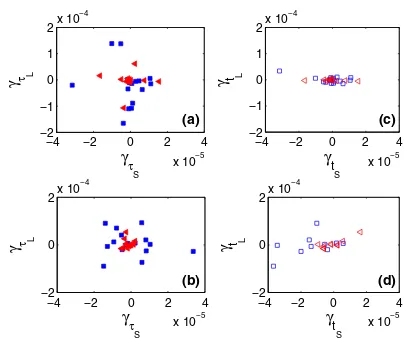
Fig. 6: (Colour on-line) Scatter plots of the DAVAR scaling exponent, represented byµt(τ), for normal (circles) and CHF (diamonds) subjects: (a) short term, (b) long term, (c) short scale, and (d) large scale.
higher dispersion than for CHF patients, indicating that on average the variation of σy(t, τ) from one time(scale)
to another, for a given scale(time), is more dependent on the value of scale(time). In contrast, the corresponding average values for CHF patients have lower dispersion. Thus, the local stability for heart interbeat of normal subjects tends to change in time and scales differently with respect to the time and scales, than for CHF patients for which a more regular evolution of stability in time and scales is observed.
Furthermore, for analyzing the scales and time evolu-tion, we compare the value of both µt(τ) and γτ(t) for
selected combinations of scales and time. For instance, for the short-term (standing at the first analysis window) and the long-term (last analysis window), we pick values of µt(τ) for short (µτS) and large (µτL) scales (figs. 6(a)
and (b), respectively). Similarly, for the shortest and the largest scales, we pick values for the short (µtS) and the
long (µtL) terms (figs. 6(c) and (d), respectively). The
same approach is applied to γτ(t) (fig. 7). For the
scal-ing exponent µt(τ) (figs. 6(a) and (b)), we observe that
for healthy subjects the values for the small scales are slightly larger than for large scales; while for CHF patients the values from small scales are quite larger than for large ones. The values ofµt(τ) for healthy subjects are
signifi-cantly different than for CHF patients (p-value<0.05 by t-Student test). For small-scales (fig. 6(c)), the scaling expo-nents are almost over the identity line for both groups indi-cating low variation with time. Moreover, for the healthy group the scaling exponents are positive, while for the CHF group is the opposite. For large scales (fig. 6(d)), the scaling exponents are more spread. For the variation in time for DAVAR, expressed by γτ(t), we observe for
short and long terms (figs. 7(a) and (b)) a cluster around zero for CHF patients (specially for the short term), while for normal subjects the values are spread. In this case, we have not found statistical difference between both groups.
−4 −2 0 2 4
x 10−5 −2
−1 0 1 2x 10
−4 γ τ S γ τ L (a)
−4 −2 0 2 4
x 10−5 −2
0 2x 10
−4 γ τ S γ τ L (b)
−4 −2 0 2 4
x 10−5 −2
−1 0 1 2x 10
−4 γt S γ t L (c)
−4 −2 0 2 4
x 10−5 −2
0 2x 10
−4 γt S γ t L (d)
Fig. 7: (Colour on-line) Scatter plots of the time variation of DAVAR, represented byγτ(t), for normal (squares) and CHF (triangles) subjects: (a) short term, (b) long term, (c) short scale, and (d) large scale.
A similar clustering around zero is observed also for CHF patients for values corresponding to small and large scales (figs. 7(c) and (d)). For healthy subjects, the values for small scales are also clustered although at a less extent, however, at large scales they are spread out at a higher extent than for CHF group.
Discussion. – Some previous studies have approached heart interbeat by using the so-called Allan factor, based on AVAR, calculated over the number of beats counted in boxes of lengthT, considering the heart beat dynamics as a point process [6,10]. However, the approach followed in these studies does not take advantage of the property of the AVAR to quantify the frequency stability of an oscil-lator. Moreover, the previous studies did not perform a dynamicanalysis, i.e., an investigation of the time evolu-tion of stability. The stability of a frequency standard, as quantified by AVAR, tells us the deviation of the oscil-lator’s frequency from its nominal value, at a certain observation period (scale)τ. Thus, a low value of AVAR indicates a more precise frequency standard (more stable oscillator), and also the variation of AVAR for different scalesτ indicates the behavior of the stability.
We found three scaling regions for the DAVAR for the healthy group and four for the CHF group, where the first two regions are delimited by inflection points at around the same scale (number of interbeat intervals). However, the values of the time-averaged scaling exponent µt in
each of these regions are remarkably different between the groups. The behavior is opposite between the groups in the first two regions, while in the third one, the values of µt for the normal group decreases linearly, while for
the CHF group they increase up to an inflection point, after which they remain approximately constant. After the inflection point atk∼60, the values ofµtare
nega-tive and decrease monotonically, indicating that the stabil-ity of the interbeat rate for the normal group increases.
[image:7.595.63.266.80.243.2] [image:7.595.322.524.81.250.2]R. Hern´andez-P´erezet al.
On the contrary, for the CHF group the values of µt
increase to reach positive values, indicating a degradation in stability of the interbeat rate. Previous studies have reported different scaling regimes for healthy and heart-failure subjects in sleep and wake phases, with a noticeable cross-over at≈60 beats [20]; strongly suggesting that the scaling characteristics in the heartbeat fluctuations during sleep and wake phases are related to intrinsic mechanisms of neuroautonomic control. The several scaling regions reported in the present work support the hypothesis of the presence of intrinsic mechanisms of neuroautonomic control, discarding that these scaling differences are due to environmentalnoise, which can be treated as a trend and distinguished from the more subtle fluctuations that may reveal intrinsic correlation properties of the dynamics [20]. Moreover, the evolution of the DAVAR profile for both groups is captured by the scatter plots forµt(τ) andγτ(t).
For a stationary signal, we would expect to see a cluster around a certain value of µt(τ). However, if the signal
had different nonstationary features or correlated compo-nents, there would be larger dispersions or deviations from the identity line in the scatter plots. However, regarding parameterµt(τ), we observe that for healthy subjects the
scaling exponent for the small scales is slightly larger than for large scales; while for CHF patients we identify two regions with opposite behaviors. Thus, CHF signals have stochastic components close to white noise. These compo-nents dominate for small scales for which it corresponds a lower value of the scaling exponent (close to−0.5), which is consistent with other approaches [7]. This is not the case for healthy subjects, for which more long-correlated components are present, whose scaling exponent is larger.
Conclusions. – We map the heart to an oscillator and then we perform a stability analysis of the heart interbeat interval rate, using tools developed for the characterization of the frequency stability of frequency standards. In particular, we employ the dynamic Allan variance (DAVAR) to analyze heart interbeat time series for normal subjects and patients with CHF. We find that DAVAR can discriminate the heart interbeat dynamics between both groups. Moreover, the evolution of stability in scales and time is revealed by DAVAR and its numerical partial derivatives. We consider that the DAVAR can contibute to the study of heart interbeat, not only for its computational simplicity but also for its ability to quantify the local stability and to reveal the nonstationarities in the signals. For making it useful for clinical usage, further work has to be performed to characterize the DAVAR profiles for several cardiopathies.
∗ ∗ ∗
We thank L. Galleani for helpul advice and discus-sion; and the anonymous referees whose suggestions led to
improvement of the manuscript. This work was partially supported by CONACYT (Grant 49128-F-26020), COFAA-IPN, EDI-IPN, M´exico.
REFERENCES
[1] Ivanov P. C., Amaral L. A. N., Goldberger A. L., Havlin S., Rosenblum M. G., Stanley H. E. and Struzik Z. R.,Chaos,11(2001) 641.
[2] Ivanov P. C., Amaral L. A. N., Goldberger A. L., Havlin S., Rosenblum M. G., Struzik Z. R. and Stanley H. E.,Nature,399(1999) 461.
[3] Goldberger A. L., Amaral L. A. N., Hausdorff J. M., Ivanov P. C., Peng C. K. andStanley H. E., Proc. Natl. Acad. Sci. U.S.A.,99(2002) 2466.
[4] Kantelhardt J. W., Ashkenazy Y., Ivanov P. C., Bunde A., Havlin S., Penzel T., Peter J.-H. and Stanley H. E.,Phys. Rev. E,65(2002) 051908. [5] Karasik R., Sapir N., Ashkenazy Y., Ivanov P. C.,
Dvir I., Lavie P.andHavlin S.,Phys. Rev. E,66(2002) 062902.
[6] Turcott R. G.andTeich M. C.,Ann. Biomed. Eng.,
24(1996) 269.
[7] Guzm´an-Vargas L., Calleja-Quevedo E. and
Angulo-Brown F.,Fluct. Noise Lett.,3(2003) 83. [8] Schmitt D. T.andIvanov P. C.,Am. J. Physiol. Regul.
Integr. Comp. Physiol.,293(2007) 1923.
[9] Guzm´an-Vargas L., Mu˜noz-Diosdado A. and
Angulo-Brown F.,Physica A,348(2005) 304. [10] Viswanathan G. M., Peng C. K., Stanley H. E. and
Goldberger A. L.,Phys. Rev. E.,55(1997) 845. [11] Ivanov P. C., Rosenblum M. G., Peng C.-K., Mietus
J., Havlin S., Stanley H. E. andGoldberger A. L., Nature,383(1996) 323.
[12] Reyes-Ram´ırez I. and Guzm´an-Vargas L., EPL, 89
(2010) 38008.
[13] Allan D. W.,IEEE Trans. Ultrason. Ferroelectr. Freq. Control,34(1987) 647.
[14] Rutman J.,Proc. IEEE,66(1978) 1048.
[15] Galleani L. and Tavella P., IEEE Trans. Ultrason. Ferroelectr. Freq. Control,56(2009) 450.
[16] Bernaola-Galv´an P., Ivanov P. C., Nunes Amaral L. A. and Stanley H. E., Phys. Rev. Lett., 87(2001) 168105.
[17] Percival D. B. and Walden A. T.,Wavelet Methods for Time Series Analysis (Cambridge University Press, New York) 2000.
[18] Ivanov P. C., Nunes Amaral L. A., Goldberger A. L. and Stanley H. E., Europhys. Lett., 43 (1998) 363.
[19] Goldberger A. L., Amaral L. A. N., Glass L., Hausdorff J. M., Ivanov P. C., Mark R. G., Mietus J. E., Moody G. B., Peng C.-K.andStanley H. E., Circulation,101(2000) e215.