www.elsevier.es/rmuanl
EXPERT’S
CORNER:
A
PERSONAL
APPROACH
Migraine
management
A.
Marfil
∗HeadacheandNonOncologicPainClinic,NeurologyServiceattheUniversityHospital,‘‘Dr.JoséEleuterioGonzález’’of theUniversidadAutónomadeNuevoLeón,Mexico
Received12February2015;accepted24February2015 Availableonline11June2015
Introduction
Migraines are common illnesses. Studies conducted in 12 LatinAmericancities,includingtwoinMexico,havefound thatitsprevalenceinourcountryis15%.Therateingender is3:1(Women/Men)worldwide.
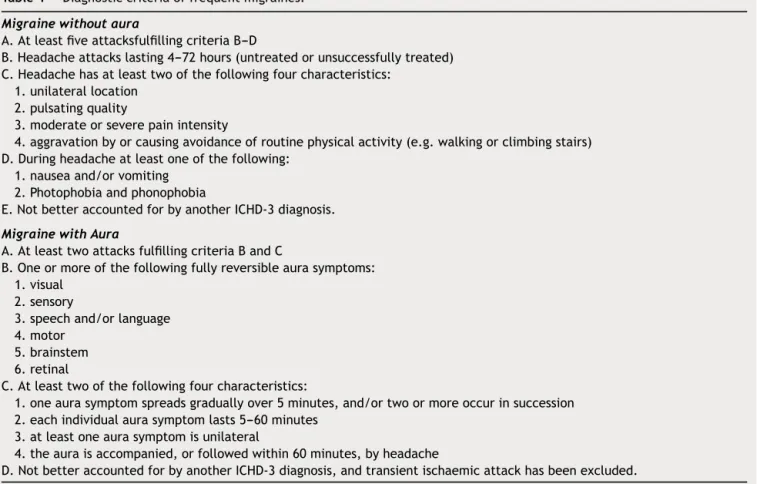
Thediagnosticcriteriaformigraineswerepublishedfor thefirsttimein1988,inthefirsteditionoftheInternational Headache Classification, promoted by the International Headache Society, with its second edition in 2003, and a third beta version that will probably be published in 2015.Diagnosticcriteriaforthedifferentformsofmigraines werefirstdescribedinthisdocument,whichhassimplified communicationamongdoctorsandmadepossible compar-isonsbetweenstudies.Thecurrent migrainecriteria(with andwithoutaura)areshowninTable1.
Asinallprimaryheadaches,paraclinicandimaging stud-iesarenormalandrarelynecessary,exceptionmadeforthe caseswherethereisclinicaldoubtorwheneverthepatient istooanxiousandwishestobe‘‘ascertainasyoucanbe’’. Thismaybeavalidreason;howeveritmayincreasethecost ofmedicalattentionandcanbeproblematicininstitutions withahighvolumeofpatients.
The management of migraines must contemplate two aspects:
1. Acutemanagement(abortive). 2. Preventivemanagement.
∗Corresponding author at: Servicio de Neurología del Hospital
Universitario ‘‘Dr. José Eleuterio González’’, de la Universidad AutónomadeNuevoLeón.Av.MaderoyGonzalitoss/nCol.Mitras Centro,MonterreyC.P.64460,N.L.,Mexico.Tel.:+528183471059.
E-mailaddress:amarfil1@yahoo.com
In both cases, the following pharmacological and non-pharmacologicalmeasuresmustbecontemplated.
Management
generalities
Beforebeginningmanagementofamigraine,asinanyother pathological entity, we must ask ourselves, several ques-tions:
1. Aremedicationsnecessary?
2. Ifso,arethereparameterstochooseoneasthebest? 3. Howwillresultsbemeasured?
4. Whichwillthesuccess andfailurecriteriabetodecide achange in management?In other words,how longto maintainamedicationbeforeconsideringitdidnotwork. 5. Howlongwillasuccessfultreatmentlast?
6. Whatistheaprioriprobabilityofrecovery/recurrence?
Answeringeachandeveryoneofthesequestionsbefore
beginning management is fundamental. It gives the man-agement sense anddirection, for both the doctoras well asthepatient.Additionally, itbringsthepatientthe feel-ingthathe/sheisabletodosomething,orcooperateinthe treatment,andthusthepatientperceiveshe/shehassome controloverhis/herillness.
Abortive
management
Generalguidelines:
1. Totreatasearlyaspossible.Theinstructionis:‘‘Takethe medication, or doasindicated, assoon asthepatient
recognizes if a crisis arises.’’ Patients learn to
recog-nize when this happens, and we know that abortive
http://dx.doi.org/10.1016/j.rmu.2015.05.001
Table1 Diagnosticcriteriaoffrequentmigraines.
Migrainewithoutaura
A.AtleastfiveattacksfulfillingcriteriaB---D
B.Headacheattackslasting4---72hours(untreatedorunsuccessfullytreated) C.Headachehasatleasttwoofthefollowingfourcharacteristics:
1.unilaterallocation 2.pulsatingquality
3.moderateorseverepainintensity
4.aggravationbyorcausingavoidanceofroutinephysicalactivity(e.g.walkingorclimbingstairs) D.Duringheadacheatleastoneofthefollowing:
1.nauseaand/orvomiting 2.Photophobiaandphonophobia
E.NotbetteraccountedforbyanotherICHD-3diagnosis.
MigrainewithAura
A.AtleasttwoattacksfulfillingcriteriaBandC
B.Oneormoreofthefollowingfullyreversibleaurasymptoms: 1.visual
2.sensory
3.speechand/orlanguage 4.motor
5.brainstem 6.retinal
C.Atleasttwoofthefollowingfourcharacteristics:
1.oneaurasymptomspreadsgraduallyover5minutes,and/ortwoormoreoccurinsuccession 2.eachindividualaurasymptomlasts5---60minutes
3.atleastoneaurasymptomisunilateral
4.theauraisaccompanied,orfollowedwithin60minutes,byheadache
D.NotbetteraccountedforbyanotherICHD-3diagnosis,andtransientischaemicattackhasbeenexcluded.
treatmentloseseffectinadirectproportiontothedelay intreatment.
2. Tohave a recordof theamount of analgesic used.Set limitsandhavea‘‘planB’’and‘‘planC’’readyincase ofacutetherapeuticfailure.
3. Ifwe aregoingtotryamedication (i.e.atriptan),try it in at least two crises before declaring therapeutic failure.
4. Rememberthattheabortivetreatment isexactlythat: abortive.Althoughthereareexceptions;itmustnotbe used with a schedule. The principle is to NEVER give abortivemedicationonaschedule.Exceptionswouldbe situationswherewecananticipatetheonsetofthecrisis, likemigrainesassociatedwithmenstruation(with regu-larcycles)orepisodicclusterheadache.Ingeneral,the evolutionofthecrisis inmostmigrainesispredictable; thus the patient is able to know when to take the medication.
Non-pharmacologicalmeasures
Somepatientslearnsometechniqueswhichcanhelp attenu-atethepainormakeitdisappear.Themostutilizedmethod issleep.Thephysiciancantrytocompressbothsuperficial temporalarteriesinfrontofthetragus(oronthesidewhere thereispain,ifitishemicranial)inordertotrytoabortthe
crisis.Itseffectivenessisestimatedtobebetween30%and 40%.
Dietis reservedfor thosecases wherethereis a close
temporalrelationshipbetweenthedietaryelementimputed
and the onset of the crisis. There is no point in giv-ing a restrictive diet a priori. The idea of prohibiting theconsumption of specific food,like chocolate, cheese, cannedfoods,sausages,Chinesefood,wine(especiallyred) or any form of alcohol, among others, is highly popu-lar. The experience in ourcenter is thatfood trigger are rare.
A careful interrogatory is the best tool to indicate a restrictive diet. Therefore, it is mandatory to keep a headache diary where the patient must record the number of attacks, intensity, time, response to medica-tions, and relationship to external events or foods. This diary will give us the parameters to make changes in management.
Medications
However,thereisnowayofpredictingtheresultofa partic-ularmedicationinaparticularpatient.Furthermore,failure ofonetriptandoesnotpredictthefailureofanother,thus trying out two or three different triptans may be justi-fied. Our protocol is to start with one of these two, to try it for at least 2 crises, and decide whether or not theyworked. If they did not work, switch to a different triptan. The instruction to the patient is: take (or place the wafer of rizatriptan or zolmitriptan over/under the tongue) themedication assoon as thepatient recognizes
theonsetof a crisis. Keep in mindthat theeffectiveness ofthe medicationdecreases withtheintervalbefore tak-ingit;oncethefirstdosage ofmedicationistakenweask them to wait for an hour; if at the end of the hour the crisis is not over, take the second dose. If after the sec-ond hour (an hour after the second dose), the crisis has notdisappeared, begin witha second, different, medica-tion. The concept of ‘‘crisis disappearance’’ is precisely that: tocompletely stop not only the pain(which should completely disappear), but also the autonomic and cog-nitive symptoms, etc. If residual symptoms persist, the probabilityof recurrenceisgreater. Recurrenceisdefined as the reappearance of a crisis in a period shorter than 24hfromtreatment. Itis importanttorememberthatall abortivemedications,ifusedfrequently,cancauserebound headaches.Thustheneedtokeeptrackofanymedication thatthepatientmaytake,eveniftheyareover-the-counter medications.
Ergotamine is also effective and low-cost, making it a good option for institutions with a high volume of patients.It hasan effectivenessof 40---60%in pain reduc-tion/disappearance.The main problem is that itis highly addictive and we must take all precautions when utiliz-ingpotentially addictivedrugs: keeptrackof medication, superviseprescriptions,andreviewresultsfrequently. Indi-cationstothepatientare:initiatetreatment assoon asa crisisisrecognized;startwith1mgofthe usual presenta-tions(twotabletsof0.5mg)andgivean additional0.5mg everyhalf houruntilone ofthesethreethings occur:the crisisaborts,thepatientstartsvomiting,or6tablets(3mg) aretaken.Theconsumptionofmorethan6tabletsina24h period,or 16(8mg)inaweek isthethresholdtodevelop rebound headaches, in addition to increasing the risk of addiction. If the episode ceases at, let us suppose, 2mg (fourtablets),andthepainreturnswithinthefollowing24h, medicationwillbegiventothepatient‘‘as ifitwerethe nexthalfanhour’’Iflonger,itwillbeconsideredasanew episode.
Over-the-counter medications are commonly utilized,
motuproprio, by patients. Manylearn that certain
med-ications or a combination of analgesics give them relief or abort the crisis. The problem with self-medication is that it is the singlemost important factor for chronifica-tionand the transformation of an episodic migraine toa chronicone.There willalwaysbetheneed toinvestigate the use, dosage, frequency,etc. of suchself-medication. Thesameprincipleapplieswith‘‘natural’’medicationsor herbalmedicine.Thephysicianshouldintentionallyaskfor theirusebecausetheremaybeactivepharmacological prin-ciplesthat can complicate the evolution or result of the treatment.
Table2 Levelofevidenceforpreventivemedicines.
LevelA:Medicationswithawell-establishedefficiency (≥2Class1clinicaltrials)
A.Antiepileptics:Divalproexsodium,topiramate sodiumvalproate
B.Betablockers:metoprolol,propranolol,timolol C.Triptans:frovatriptan
LevelB:Medicationsthatarelikelytobeeffective(1 class1study/2class2studies)
A.Antidepressants/SISRs/SISNRs/ATT:Amitriptyline, venlafaxine
B.Betablockers:atenolol,nadolol C.Triptans:naratriptan,zolmitriptan
LevelC:Possiblyeffectivemedications(oneclass2 study)
A.ACEIs:lisinopril B.ARAs:candesartan
C.Alphaagonists:clonidine,guaifenesin D.Antiepileptics:carbamazepina E.Betablockers:nebivolol,pindolol F.Antihistamines:cirpoheptadina
LevelU:Insufficientorinadequatedatatomake recommendations
A.Carbonicanhydraseinhibitor:acetazolamide B.Antithrombotics:acenocoumarol,coumadin, picotamide
C.AntidepressantsSISRs/SISNRs:fluvoxamine, fluoxetine
D.Antiepileptics:gabapentin E.Tricyclics:protriptyline F.Betablockers:bisoprolol
G.Cachannelblockers:nicardipine,nifedipine, nimodipine,verapamil
H.Vascularsmoothmusclerelaxants:cyclandelate
Other:Medicationsestablishedaspossibly/probably ineffective
A.Establishedasineffective:lamotrigine B.Probablyineffective:clomipramine
C.Possiblyineffective:acebutolol,clonazepam, nabumetone,oxcarbazepine,telmisartan
ACEIs: angiotensin converting enzyme inhibitors; ARAs: angiotensinreceptorantagonists;SISRs:selectiveinhibitorsof serotoninrecovery;SISNR:selectiveinhibitorsofserotoninand norepinephrinerecovery.
Itisimportanttokeepinmindthattheidealobjectiveof treatmentisnottouseabortivemedications,becausethere arenomoreepisodes.
Itisimportantnottomixergotaminesandtriptansinthe samesessionoftreatment.Itisaparamount contraindica-tionthatonemustkeepinmind.
Preventive
treatment
theirlevelsofevidencefromtheAmericanAcademyof Neu-rologyguidelines,1 that ingeneralagreewiththe restof
internationalorganizations.
In our country there is no hard data on the effec-tivenessof medicationsin our population, however there is some useful information. In 2005, the Headache Study Group of the Mexican Academy of Neurology published a consensus on the management of migraines. Combin-ingexperiences,weproposedthatourpopulationrequired lowerdosesthanthosepublished.Thisdatahasbeen com-mented on international meetings and our colleagues in LatinAmericaandSpainconcurwiththeimpressionthatthe doses generally needed in our respective populations are lower. Regarding the preferences of medications,in 2008 ourgroup conductedanational surveyonthebehaviorof neurologists andneuropediatriciansinthemanagementof migraines.2
Nonpharmacologicaltreatment
Asmentionedabove,onemustidentifytheindividual trigg-ering factors, should there exist. Even though they are not very frequent, they can be: dietary elements, lack or excess ofsleep,irregular mealtimes, andexposure to intense light. The causal relationship between stress and the production of a crisis is hard to prove, even if it is an idea that ‘‘sounds good’’. Obesity has been proven as a risk factor for migraine chronification and dimin-ished response to medication. Thus it is recommended, as in other situations, to comply with general rules of hygiene.
Preventivemedications
InTable2thereisalistofmedicationswithbetterevidence. Therecommendationsfornon-neurologistsare:
1. Alwayskeepa‘‘headachediary’’recordingthenumber of crises, intensity, duration, time, associated symp-toms,triggers, effectof usedmedications,unwanted oradverseeffects,needofrescuemedicationanddays withoutpain.It isfundamental in ordertoassess the result of the treatment. Aside from this, the MIDAS scalecan beusedtoassesstheimpactof thedisease onactivitiesofdailyliving.
2. There arenospecific guidelines or criteriatostart a preventivetreatment.Ingeneral,wetakeintoaccount thenumberofcrisesandtheimpactonqualityoflife. Withtwoormorecrisespermonththerisk/benefitratio ofmedicationsisconsideredsatisfactorytojustifythe beginning of treatment. In some people (i.e. women withmigrainesassociatedwithmenstruationand reg-ular cycles) we are able to begin ‘‘short preventive treatments’’,threedaysbeforeandaftertheexpected onsetofthecrisis,ineachcycle.Thesamehappensin othertypesofheadacheswhereweareabletopredict theonsetofacrisis.
3. Learntomanagetwoorthreemedicationswell. Prefer-ablyfromtwodifferentgroups.
4. Consider comorbidities. Rule out if the patient is hypertensive,suffersfromasthma,anxiety,depression, obesity or other conditionsthat may indicateor con-traindicateaspecificmedication.
5. Encourage the patient to comply with non-pharmacological measures: enough sleep, regular mealschedules,weightloss,regularexercise,avoiding excessesoffood,drinksandalcoholandothergeneral hygienemeasures.
6. Establish,alongwiththepatient,atreatmentplanwith specific measurable goals and commit him to accom-plishing them. The incidence of non compliance or abandonment oftreatmentsishighandshouldalways beinvestigatedineachvisit,sinceitmaybeacauseof therapeuticfailure.
7. There is not a guideline or specific evidence on the durationofasuccessfultreatment.Theintervalsvary. In our national survey, most neurologists and pedia-triciansconsideredmaintainingasuccessfultreatment for 6---8 months.However,therewere responses from 3 to 12 months. In general, a treatment is planned to last 8 months without a crisis. The first two months are useful to assess the effectiveness of the medication.
8. Atthebeginningoftreatmentweknowthereisa prob-ability of effectiveness.We mustmaintain theuse of a medicationfor atleast twomonthsat properdoses beforedecidingitisnotworking.Afrequentcauseof ‘‘treatment failure’’ is not giving it enough time to work. This shouldbe clearlyexplainedtothepatient sothathe/shecooperatesduringthisperiodandexert enoughpatience.
9. Attheendoftheplannedperiod,stopthemedication andobserve.Therateofrecurrenceis30---40%. 10. Whilethegoaliszerocrises,sometimesafewmaybe
tolerated,eitherbecauseoflowtolerabilityofthe med-icationor becausethepatientisreluctanttoincrease the dose. In these cases there are no specific num-bersaboutthe cure/recurrencerateaftercompleting a treatment. We must explain to the patient that migraines arediseasesthat tend torecurindifferent epochsinlife.
11. In case of recurrence after a successful treatment (monthsor yearslater),themost reasonable thingto doistorestartthetreatmentwhichwasuseful.
Migrainesareacondition whichcanbecontrolledand, sometimes ‘‘cured’’. We ought to understand that the concept of curing is similar to that of other chronic conditions of difficult prognosis (rheumatics, oncological, etc.), which is the absence of recurrence in a deter-minedperiod of timeafter treatment. The doctor should pay attention to the details of the treatment in order to communicate to the patient what he is trying to be accomplish, and thus be able to gain his trust and cooperation.
Conflict
of
interest
Funding
Nofinancialsupportwasprovided.
References
1.Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Evidence-based guideline update: pharmacologic
treatmentforepisodicmigrainepreventioninadults.Reportof theQualityStandardsSubcommitteeoftheAmericanAcademy ofNeurology and the American Headache Society.Neurology. 2012;78:1337---45.