www.elsevier.es/rmuanl
REVIEW
ARTICLE
Benign
Intracranial
Hypertension
(Cerebral
Pseudo-tumor)
This
was
the
first
article
published
in
medicina
universitaria
in
January
of
1970
夽Melvin
Greer
a,
Ricardo
Rangel-Guerra
b,∗aHeadoftheDepartmentofNeurology,UniversityofFlorida,Florida,UnitesStates
bFellowChiefofNeurologyoftheFacultyofMedicineoftheUniversityofNuevoLeón,Monterrey,Mexico
Availableonline2July2015
Benign intracranial hypertension (BIH) is a neurological syndrome of diverse etiology and obscure pathogenesis. It is also called Cerebral Pseudo-tumor, serous meningi-tisorotitic hydrocephalus1.Diagnosiscan beestablished
onlyafterotherintracranialhypertensioncauseshavebeen excluded,suchasintracranialinfection,encephalopathyor atumor-relatedinjury.Thesyndromeimpliesaclinicalstate where there areno focal neurological symptoms and the patient’sstateofmindisunaltered.Theexacttreatmentis notestablishedin adefinite form,sequelaeof thisillness arenotfrequentandtheprognosisisgenerallygood.
A large variety of nosologic entities have been found in association with this syndrome. Obesity has been recognized in 14 to 59% of the reported patients in different series 4. It has been observed to be
accompa-niedby someendocrinological statesincludingpregnancy, irregular menstruation with galactorrhea, premenstrual edema,hypoparathyroidism,adrenalinsufficiencyand ther-apy with corticosteroids 8---10,13. This same syndrome has
been attributed to vitamin A intoxication 14. It has been
observedinpatientswithSydenhanchoreaandinadolescent women with microcytic and hypochromic anemia. Benign
夽 This article is a reprint of the article ‘‘Benign Intracraneal
Hypertension(CerebralPseudo-tumor)’’publishedinMEDICINA UNI-VERSITARIA,Vol.1,No.1,1970(MedicinaUniversitaria1970;1(1): 5-34)ontheoccasionofthe45thanniversaryofthejournal.
∗Correspondingauthor.FacultaddeMedicinadelaUniversidad
deNuevoLeón,Monterrey,MaderoyGonzalitosS/N,Monterrey,NL 64460,Mexico.
intracranialhypertensionpathogenesisinthesepatientshas notbeenexplained.
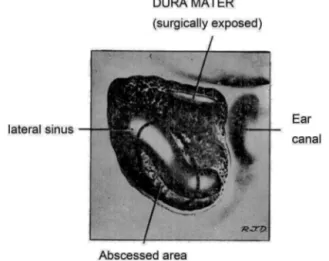
Inpatientswithmiddleearorinnerearinfection, throm-bosis of the lateral sinus has been considered the cause ofintracranialhypertension,hencetheterm‘‘otitis hydro-cephalus’’.Thrombosisofthelateralsinusinthosecaseswas identifiedduringmastoidectomyandbycarotidangiography withavenousphasestudy.
AmongstotherprobableBenignIntracranialHypertension Syndrome etiologies are aseptic cavernous sinus throm-bosis and intracranial veins. The latter lesion has been reported subsequent to a closed traumatic head injury
7, a simple skull fracture and related to pregnancy, as
well as in systemic disorders which predispose intracra-nialvenousthrombosislikecongestivevenousheartfailure, cachexia, hyperpyrexia, dehydration and the post-partum state.However,inthesepatientsintracranialhypertension wasnotbenign,withauniversallyfatalevolution. Intracra-nial venous and sinus thrombosis in said cases frequently lead to cerebral infarction, with concomitant neurologi-calfocalsignsandseizures,insteadof benignintracranial hypertensionsyndrome.
Furthermore, this diagnosis is questionable in infants with high intracranial pressure syndrome which is attributable to acute vitamin A intoxication; to ther-apy with tetracyclineand chlortetracycline, or tosudden exanthema.Inthislastsituation,thepresenceoffeverand the resolution of hypertension signs and symptoms after diagnostic spinal tap, suggest the term ‘‘meningismus’’. Meningismus is thought to be caused by a fast dilution
http://dx.doi.org/10.1016/j.rmu.2015.05.004
of the blood at the onset of fever, making it hypotonic in relation to the cerebrospinal fluid. As a result of this osmotic difference, the CSF volume may increase and temporarilyraiseintracranialpressure15.
In one patient, the syndrome was believed to have occurredasa resultof an allergicorhypersensitivity pro-cess,duetothecloserelationshipbetweentheexacerbation of headache after the ingestion of allergic medications and the improvement of symptoms within a period of 12hoursaftertheinstitutionofantihistaminicmedications
11.However,in thisparticular case therewasahistoryof
pneumococcalmeningitis,whichcastsdoubtsonthe mean-ingoftheprobableallergicprocess.
Forabetterunderstandingofthissyndrome,the expe-rience is presented with 102 patients studied at The Neurological Institute of New York and the University of Florida.
Patient
selection
Usingthefollowingcriteria,aselectionof102patientswas made,15ofthemseenpersonally:
1. Riseofintracranialpressuremanifestedbypapilledema and confirmed by measurement of cerebrospinal fluid pressurewithawatermanometer.CSFpressurewasnot registered in30 patientswho underwentneurosurgical procedures(ventriculography, subtemporal decompres-sion,andcraniotomy)butthesubsequentdisappearance ofpapilledemaconfirmedtheimpressionofintracranial hypertension.The absenceof alterations to thevisual function excluded the presence of optical neuritis in these30patients.
2. Exclusion of the possibility of an intracranial space-occupying lesion, infection of the central nervous system, toxic encephalopathy (lead poisoning), hyper-tensivevasculardiseaseandobstructivehydrocephalus, throughtheuseofproperneurodiagnosticmethods. 3. Anormalstateofmentalfunctions.
4. Absenceofseizuresandfocalneurologicalsymptoms. 5. Normal CFSglucoseand CSFcell count.This data was
necessarytoexclude,asmuchaspossible,patientswith viralinfectionsofthenervoussystemorthosewhowere sickwhere the use ofantibiotic therapy raised doubts about a possible abscessformation or thepresence of partially-treatedbacterialmeningitis.
Of the total group,64 were women and 38men; ages rangedbetween25and56years;39patientswereadmitted directlytotheprivateneurosurgicalserviceandthe diagnos-ticandtherapeuticuseofthesepatientswasoftenguidedby thepersonalexperienceoftheneurosurgeonondutyrather thanbyanyspecificdifferenceinthesignsandsymptomsof thosepatientstreatedmedically.
The 102patientsweredividedinto6categories,taking intoaccounttwocommonfactorsintheirclinicalevolution andphysicalexamination.Thecategorieswere(Table1):
Thirteenchildren,rangingfrom3to13yearsofage, suf-fered from BIH linked to an active middle and inner ear infection.Theyalldisplayedthesamesignsandsymptoms of an otic pathology during the month previous to their
Table1 BIHEtiology.
Middleandinnerearwithmastoiditis. Therapywithcorticosteroids. Lightclosedheadtrauma. Pregnancy
Suspicionofmetabolicorendocrinealterations. Miscellaneousandnon-relatedtothepreviousdata.
admission.Onlyonechildwithahistoryof5yearsof inter-mittentotorrhea was able to be considered as a case of chronicotitis;5ofthemhadbeentreatedwithantibioticsat theonsetoftheinfection,butthedurationofthetreatment wasalwayslessthan5days.
Theywerealladmittedwithinthefirstweekofthefirst symptomsofintracranialhypertension:headache,nausea, vomiting,dizzinessanddiplopia.Only3childrendisplayed feveratthetimeofadmission(37.5◦ to38.5◦ C).None of
themhadclinicaldataofdehydration.Middleearinfection (rightear)wasobservedduringtheostocopicexaminationof 11childrenandintheleftearintwoofthem.Fivechildren presentedsensitivitytopressureinthemastoidregion.13 children presented papilledema and 9 presented external oculomotorparesis.Regardingtheinjuredear,paresisofthe cranialnerveVIwasipsilateralin3patients,contralateralin 1andbilateralin5.Therewasnoothercranialnervealtered norwasthereevidenceofthrombosisinthecavernoussinus. The electroencephalogram (EEG) showed a mild focal bradyarrhythmia in the temporal or occipital ipsilateral derivationsin5 ofthepatients. Threechildren presented moderate leukocytes (13,000 to 20,000) and accelerated ESG.Radiologicaldataofmastoiditiswasfoundin11outof the13children.Allthesepatientspresentedanincreasein CSFdemonstratedbyalumbarpuncture(of220to600mm of water).Carotid pneumoencephalography and angiogra-phy were performed in 10 cases. The venous phase of thearteriogram showedobstruction of the lateral venous sinus ipsilateral to the affected ear in two patients and establishedthepresenceofventriclesofnormalsize. Pneu-moencephalographyintherest of thepatientwasnormal
(Figure1).
Otherrelevantfindingsincludedthepresenceofnormal or‘‘low’’ valuesinCSFproteins. Anelevated Ayalaindex wasfoundin6outofthe8patientswhoweremeasured.*The
elevatedindexinthese6patientsremainedthiswaywhen measuringrepeatedlyfor2weeksto6months.Bythistime thechildrenwere asymptomaticandthe papilledemahad decreasedordisappeared.However,CSFpressureremained above200mmofwater,whichiscompatiblewithanincrease involume,justasanincreasedAyalaindexsuggests.
Treatment includedmastidectomy, antibiotics, subtem-poral or suboccipital decompression, repeated lumbar punctures and anticoagulants. During the mastoidectomy thepresenceofpurulentandnecroticmaterialcoveringthe
∗TheAyalaIndexisobtainedbymultiplyingthefinalCSFpressure
Figure 1 Benign intracranial hypertension. Venous phase carotid angiogram ona 6-year-old boy with mastoiditis. The lateralprojectionshowsadistentionofthesuperficialcortical veinsandobstructionofthelateralsinusatthepointinwhich itreachesthesigmoidsinus.
Figure 2 Benign intracranial hypertension. Outline of the
findingsofthemastoidectomyof10 patientswithmastoiditis andbenignintracranialpressure.Theareaofthesinus obstruc-tionislabelledunderthename‘‘AreaofAbscess’’.
lateralsinuses andsigmoidwasobservedin everypatient.
(Figure 2) After palpation and needle aspiration it was
concluded that 2 patients had lateral sinus thrombosis; compressionofthelateralsinusandsigmoidwasdetectedin theremaining8.Aftertheextractionofthenecrotic mate-rial, the sinuses were filled and patents appeared during thecourseof8years.Inoneofthetwopatientswith possi-blethrombosis,theinternaljugularveinwastiedoffatthe jugularbulblevel.Intheotherpatientthenecrotic mate-rialcoveringthevenoussinuswasremovedandtherapeutic withanticoagulantswasinstituted.
Right subtemporal or sub-occipital decompression was performed in 4 patients. This was the only therapeutic
measure in 3 of the patients. In the fourth patient a mastoidectomy, a repeated lumbar puncture and therapy with anticoagulantswere also performed. In this particu-lar patient, at the moment of decompression, the brain herniated through the incisionof the dura mater, making alobectomynecessary.Withtheexceptionofthispatient, whosepapilledemaandintracranialhypertensionsymptoms didnotrespondtoothertherapeuticforms,thedecisionof performingasurgicaldecompressionintheother3patients wasmadewithoutprevioustreatmentorobservation.
At thetime of ventriculography or surgery itwas con-cluded that the subarachnoid space was ‘‘dilated’’ in 5 children.Withtheinfluenceofthearachnoid,CSFflowedout withpressureandthebrain,innormalappearance,seemed to re-introduce itself into the cranial cavity. After mas-toidectomy,andbecauseofthepersistenceofpapilledema orintracranialhypertensionsymptoms,3lumbarpunctures wererequired.AconsiderableamountofCSFwasextracted withthisprocedure,largeenough(10to30cc.)toreduce thetensionlevelstonormal(80to140mm ofwater).The inadequacy of this procedure was evident when a subse-quent lumbar puncture, performed 24 to 48hours later, revealed a CSFpressure equal or higherthan the original level. One child who underwent a mastoidectomy and 3 lumbarpunctureswasdischarged2½weeksafterhis
admis-sion,assoonashewasasymptomaticandtheedema had disappeared.However,thispatientwasre-admittedtothe hospitalaweeklaterasaresultofaheadacheand progres-sivepapilledema.Hewasadministeredatotalof38lumbar puncturesinaperiodof6months.
Subsequentneurologicalexamswerenormalin7patients who were monitored for a period of 1 to 5 years and 6 patientswhoweremonitoredforayear.
Light
‘‘closed’’
head
trauma
Ninemalepatients,withagesrangingfrom25to45years, sufferedalightclosedheadtrauma,adayto2weeksbefore theonsetofintracranialhypertensionsymptoms.Theperiod oftimebetweentheonsetofthesymptomsandits admis-sionwithBIHfluctuatedbetween2daysand10months.The traumacausedamomentary lossofconsciousnessinsome patients;itwasassociatedwithnauseaandoccasional vomi-ting;evenwhentherewasn’taskullfracture,seizuresorany otherneurologicalsymptom.
Inthreepatients,asignificantsymptomandoneofearly onsetwasblurryvision;oneofsaidpatientssufferedfrom this symptom for a period of 10 months. At the time of admission thepatientpresented opticalatrophy.The rest of them presented papilledema.In theradiological study, oneofthechildrenpresentedsutureseparationintheskull, withoutfindinganyotheralterations.TheEEDwasnormalin allpatients.CSFpressuresvariedbetween200and600mm ofwaterin6patients.CSFwasnotregisteredintheother 3patients,insteadtheyunderwenta pneumoencephalogra-phy.TheproteincontentintheCSFwasnormalinallpatients (lessthan 15mg.%in some)andtheAyala indexwas ele-vatedin 4 patientsfor whom pressuremeasurementsand CSFvolumewereobtained.
Twopatientswithvisualacuityalterationreceivedright subtemporaldecompressionwithoutanyimprovementinthe visualalteration.Thepatientstreatedconservativelywere observedwithoutusinganyothertypeoftherapy.
After studying this group of patients during different periods ranging from 6 months to 3 years, it was noted that the neurological exams repeated were normal in all patients,exceptfor2caseswhichhadapermanentvisual acuityalteration;althoughthiswasnotprogressive.
Corticosteroid
therapy
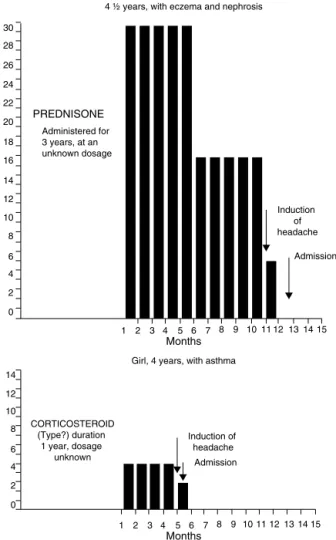
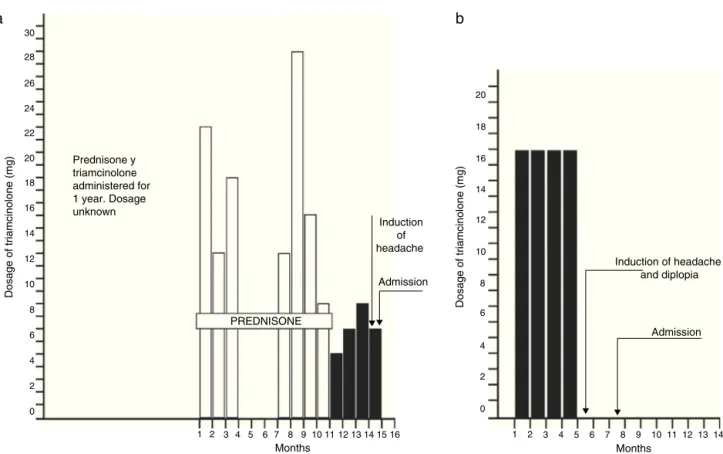
Fourchildren,between4and6yearsofage,received treat-mentwithcorticosteroidsduringvariableperiodsbetween 5monthsand3yearsbeforetheonsetofthesymptomsof raisedintracranialpressure.Theconditionsunderwhich cor-ticosteroidswereadministeredwerethefollowing:eczema in one andeczema and nephrosisin the other, asthma in thethirdandrheumaticpolyarthropathyinthefourth.The medication dosage had been reduced, practically discon-tinuedfrom1to6 weekspriortothe onsetof symptoms. Although 3 of the patients received other types of corti-costeroidmedications duringthe course ofthe conditions mentioned above, triamcinolonewasthe last preparation givento4childrenduringvariablelapsesofseveralmonths toayear.(Figs.3and4).
The patients did not display clinical signs of hypo or hyperadrenalism. Two patients displayed light atopic eczema.All4hadpapilledemaand3ofthemhaddiplopia and bilateral VI-nerve palsy. Cranial radiographies were normal in all cases. There was electroencephalographic alteration in only one patient, conscious in slow activity, moderate and diffuse, without special characters. Visual acuitywas20/200inthechildwithpolyarthropathy,aswell asinthosewhopresentedintracranialhypertension symp-tomsfor 6weekspriortotheiradmission.Sixweeksafter theirhospitaldischarge,theirvisionreturnedtonormal.
Theadrenalfunctionstudieswerenormalinonepatient (these included determinations of 17-ketosteroids and 17-ketogenicsteroids inurine anddetermination of corti-costeroidsinplasmabeforeandaftertheadministrationof intravenousACTH). CSFpressures atlumbar puncture var-iedfrom240to375mmofwaterandproteinsinCSFwere normal.
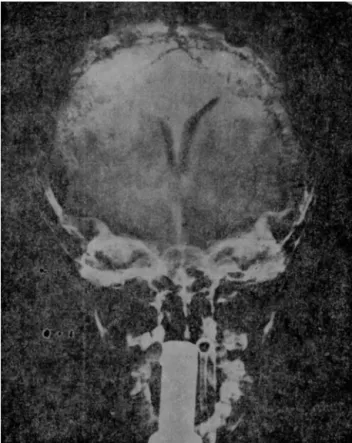
Thepneumoencephalogramwasnormalinallpatients.In onepatienttheventriculogramrevealedadecreaseinthe transversaldiameterofthelateralventricles(Fig.5).
An empiricaltreatment wasset in 2 out of 4 children with decreasing doses of hydrocortisone acetate (start-ing with doses of 25 to50mg respectively) for 3 weeks; Subtemporal decompression was performed in one of the patientstreatedinthismanner.Theother2patientswere observedwithoutanestablishedspecifictreatment.Allthe patientswereasymptomaticatthetimeoftheirdischarge; their papilledema had disappeared. It wasn’t possible to obtainanyconclusioninrelationtotheestablishedtherapy’s effect.Allchildrenwerenormalattheirfollowupayearor twolater.Onechildreceivedintermittentprednisone dur-ingthisperiodduetotherecurrenceofasthma,butdidnot showneurologicalsignsorsymptoms.
4 ½ years, with eczema and nephrosis
Girl, 4 years, with asthma
CORTICOSTEROID (Type?) duration
1 year, dosage unknown
PREDNISONE
Administered for 3 years, at an unknown dosage
Induction of headache
Admission
Induction of headache Admission
Months
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15
Months
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 30
28
26
24
22
20
18
16
14
12
10
8
6
4
2
0
8 10 12 14
6
4
2
0
Figure3 Type andduration ofcorticosteroid administered
beforetheadmissionof4patientswithBIHBoy.
Pregnancy
Eightwomen,whoseagesrangedbetween16and37years of age, were in the first semester of pregnancy at the timeof the onset of BIH. At the time of their admission theywere less than 5½ months pregnant. None of the 5
multiparouswomensufferedsimilarsymptomsduringtheir previouspregnancies.
Out of the 8 women, 4 were obese, having suffered this alteration for at least 3 years prior to their time of admission.Despite the fact that the initial symptom was theheadacheinallpatients,7ofthemcomplainedmainly about intermittent blurry vision or escotoma. There was no evidence of toxemia or peripheral thrombophlebitis. One patient had mild periorbital and pretibial edema. Papilledemawasfound in all8 patients and one of them additionally presented bilateral paralysis of the external oculomotornerve.
Prednisone y triamcinolone administered for 1 year. Dosage unknown
Dosage of triamcinolone (mg)
Induction of headache
a
b
Admission
0
2
1 3 4 5 6 7 8 9 10 1112 13 14 1516
Months PREDNISONE
2 4 6 8 10 12 14 16 18 20 22 24 26 28 30
Dosage of triamcinolone (mg)
Induction of headache and diplopia
Admission
0
2
1 3 4 5 6 7 8 9 10111213 14
Months
2 4 6 8 10 12 14 16 18 20
Figure4 (a)Boy,4½years,witheczema.(b)Girl,6years,withrheumaticarthritis.
arteriogram.In3patients,alumbarpuncturewastheonly diagnosticprocedureperformed.
Threepatients,includingtwowithalteredvisualacuity, received surgical intervention (Subtemporal decompres-sion). In one of these patients, visual acuity returned to normalvalues3weeksafterthesurgery,andremained unal-tered(20/70)intheother.
Among otherforms oftreatment, therewasthe useof ahypo-caloricdietfor the4patientswithobesity.Oneof the obese patients lost 3.157kg during her hospital stay; however,afterabandoningherdiet,re-gained3.608kgina periodof12daysandwasreadmittedtothehospitalwith recurrentpapilledemaandheadache.
Allpregnancies(exceptforone)werecompletedwithout obstetric or post-partum complications. One patient suf-feredamiscarriageaweekaftertheonsetofBIHsymptoms. 12patientswereintheir3rdtrimesterofpregnancy
(approx-imately).Afteran examination ofthe patientsabout 6 to 18monthsaftertheirhospitalization,theywereall asymp-tomaticandnormalfromaneurologicalpointofview.
Probable
endocrine
or
metabolic
alterations
Thirtyninewomen,betweentheagesof11and49yearsof age,hadBIHassociatedwithwhatcouldbeconsideredan endocrineormetabolicalteration.
A) MENARCHE.Sevenchildrenbetween11and13yearsof agebegan developing secondary sex characteristics at thetimeoftheonsetofintercranialhypertension symp-toms.Onlyoneofthemhadmenstruated,(menarche1
monthbeforeheradmission).Anothergirlhadbeen tak-ing150,000 units ofvitamin Afor aperiodof 2weeks prior to her admission. There were no dermatological signsofintoxicationcausedbyvitaminAandthelevels ofsaidsubstanceinserumwerenormal,(determined3 daysafterthedrughadbeensuspended).Onegirlwas obese.
B) MENOPAUSE. Six women, all between 40 and 49 years ofage,werebeginningtheirclimactericperiodandhad hadoccasionalperiodsofamenorrheaduringthecourse ofthepreviousyearpriortotheiradmission.Inaddition to the intracranial pressure increase symptoms which these patients presented, there were manifestations of thevasomotor type, suchas‘‘hotflashes’’,sudden increasesinsweating,intermittentflushing,etc.A sev-enth patient,a35-year-oldwoman,wasgoingthrough menopauseafterthesurgicalremovalofherpolycystic ovaries,whichhadbeenperformedapproximatelyayear beforeheradmissiontothehospital.Twooutofthesix patientswereobese.
Figure5 Benignintracranialhypertension.Ventriculography ofa4-and-a-halfyearoldboywithbenignintracranial hyper-tension, which occurredduring treatment withsteroids. The diminishment of the bodies of the lateral ventricles can be notedintheirtransversediameterintheanteroposterior pro-jection,withtheforeheadfacingup.
the 5 patients presented hirsutism and galactorrhea. Oneofthesetwopatientsbeganlactatingspontaneously whenthemenstrual flowreappeared2 daysafter hav-ingarightsubtemporaldecompressionperformed.The adrenal and thyroid function studies were normal, as wellastheexcretionofthefollicle-stimulatinghormone. The other patient, a 23-year-old obese woman, com-plainedofintermittentlactationandamenorrheafor a periodofayearandahalfpriortoherhospitalization. Neitherofthetwopatientswaspregnant.
D) OBESITY.The remaining19 patientsof thegroupof 39 were between the agesof 15 to 45 and obese.These patients,inadditiontothe4womennotedinthis cat-egory, had been overweight for at least 2 years prior totheiradmission(bodyweightrangingbetween75.600 and105.300kg).Therewereslightmenstrual irregulari-tiesin7outofthe19obesepatients,foraperiodof2to3 years,includingintermenstrualbleedingandoccasional episodesofamenorrhea.
In24outofthe39patientsthefirstandmostalarming symptomwasvisualacuityalteration.Inonepatient,visual acuitywasreducedtotheperceptionoflightwithoneeye, andwaslessthan20/70inanother6.Specialattentionwas givento3patientswithhemianopsia(theirclinicalcourseis describedlater).
Therewereradiologicalsymptomsofintracranial hyper-tensionin6ofthe39patients(erosionofthesellaturcica orposteriorclinoids);thesizeofthesellawasnormalinall cases.Therewasminimumanddiffuseslowactivityinthe EEGsof5patients; theEEGsofthe remaining34patients werenormal.Adrenal cortical functiontests werenormal inthe6patientsstudiedandthesimultaneousmeasureof serumosmolarityandCSFwerenormalin4women.
Cerebrospinalfluidlumbarpressurefluctuatedbetween 240and600mmofwaterin25outof27patients.Normal pressureswererecordedintwopatientsaftersurgery (Sub-temporaldecompression). CSFproteins werenormalinall patients (less than 15mg % in 8). In 6 patients the Ayala indexremainedelevatedforperiodsofupto3to6months afterhospitalization,wheretheyperformedrepeated lum-barpuncturesduringasymptomaticperiods.
The pneumoencephalogramwasnormal in allpatients, and in 8 cases the carotid arteriogram was also nor-mal. Subtemporal decompression was performed in 26 of the patients, including 3 whose decompression was pre-cededbyanexploratoryfrontalcraniotomy(practicedbased onsuggestiveclinical symptomsandradiologicalfindings). Anotherobesepatientunderwentasuboccipitalcraniotomy whichresulted inthedeathofthepatientafteran uncon-trollable infratentorial bleed. The autopsy revealed, in additiontothe hemorrhage, the presenceof a small aci-dophilic adenoma of the hipofisis that did not erode nor enlargethe sellaturcica. Noendocronogical studies were performed.
Out of the 12 patients who underwent subtempo-ral decompression due to visual alteration, 7 presented improvement in the visual function after surgery. This includes2patientswithhomonymhemianopsia,where sub-sequentstudiesshowedthecompletedisappearanceofthis inexplicablefinding. The remaining 5 patients withvisual abnormalitieswhoreceivedsurgicaltreatmentdidnotshow improvementofthevisualfunction.
Out of the 26 patients treated surgically, 12 were admitteddirectly tothe NeurosurgeryService, where the management of the patients was decided by the corre-sponding neurosurgeon. Complications after the surgery included focal seizures (contralateral, to decompression) in2 patients, andtransitory worseningof visualacuity in another2.
Subarachnoidspacewasfound‘‘distended’’in18ofthe operated patients. Cortical biopsies in 3 patients did not revealabnormalities.Inanother4patientsthebrainseemed toprotrudethroughtheduramater.
Seriallumbar punctureswereperformed in 12patients for periods of 1 to6 months.Improvement wasnoted in thevisualfunctionin4outofthe5patientswhowerenot treatedsurgically.CSFpressureatthelastlumbarpuncture wasstillabove200mmofwaterin9ofthe11asymptomatic patientswhosepapilledemahaddisappeared;however,the elevationofCSFpressurewasalwayslowerthanthepressure originallyrecorded.
Therefore, 47 of the 102 patients of this series were women whowere pregnant or presented signs and symp-tomsof someendocrineor metabolic change; however,it is certainly suggestive thata hormonalalteration maybe linkedtothedevelopmentofintracranialhypertension;itis notpossibletoobtaindefiniteproofofthislinkwithinthis study.
Non-related
and
miscelaneous
The remaining 29 patients constitute the heterogeneous groupof14menand15women,withagesranging from8 to58 years of age. There wereno common clinical facts thatcouldseparatethemindefinedetiologicalcategories. However,13patientssufferedfrommildextracranial inflam-matory diseases such as: paranasal sinuses infection (5), purulentconjunctivitis(3),toothabscesses(21)andanother 3patientssufferedfromrecentinfectionsoftheupper respi-ratorytract.Therearenoclinicalorpara-clinicaldata(CSF test)ofintracranialgeneralizationintheseconditions.
As observedin previous groups,visual alterationswere the most significant manifestations in 18 out of the 29 patients.
Radiologicaltestsofintracranialhypertension(erosionof thesellaturcica)werefoundin3patients;ethmoidsinusitis inthefirst,maxillarysinusitisinthesecondandfrontalin thethird.Therewereslightencephalographicalterationsin 4ofthe 29patients,translatedfundamentallyby the dif-fuseslowactivity.Therewerenoabnormalitiesintherest ofthepatients.Thestudiesofcorticaladrenalandthyroid functionswerenormalin4ofthewomen.
CSFlumbarpressureswerebetween200and600ofH2O
in17patients;therewasnoCSFregisteredfortheother12 patientssurgicallytreated;CSFproteinswerenormal(less than15mg%in4cases).
Patients treated conservatively who had a binocular vision of 20/70 improved to20/20 after repeatedlumbar punctures. Nine patients did not receive specific therapy and were asymptomatic at the time of discharge, 2 to4 weeksafterventriculography;allofthepatientswerefine 6monthsto3yearslater.
Twelveoutof twentyninepatientscheckedaftertheir hospitaldischarge(between1and17yearslater)were nor-malfromtheneurologicalpointofview,aswellastheother 17whowerecheckedforaperiodshorterthan1year.
Duration
of
symptoms
Thedurationofintracranialhypertensionsymptomswas,in general,shorterinchildrenwithoticinfection(averageof6 days).Inotherpatientsthesymptomaticperiodfluctuated, usuallybetween3weeksand2months;however,itwas dif-ficulttoevaluatethestartingdateofthesymptomsinmany patients dueto the ambiguity of their clinical manifesta-tions.In fact, 10 patientsexperienced chronic headaches andintermittentblurryvisionfor periodsbetween6to18 monthsprior to their admission. With the exception of 9 patients whowere readmitted more than 2 months after their hospital discharge, the duration of their symptoms, withouttakingtheirtreatmentintoaccount,variedbetween 2to7weeksaftertheiradmission.
Discussion
Pathogenesis
Intracranialpressuredepends ona) thevolumeordensity of the brain and spinal cord,b) CSFvolume andc) brain blood flow andintracranial blood volumeinside the cran-iospinalvault.Anincreaseinoneofthesefactorsresultsin anincreaseinthepressureinsidethisvault,unlessthereis a compensatorydescentof oneof thetworemaining fac-tors.Theinadequacyofthesecompensatorymechanismsin manypathologicalstatesresultsinan increasein intracra-nialpressure.
Acute and important fluctuations of blood pressure, alterations inCO2 concentrations and,toalesserdegree,
thecontentofoxygenandbloodPh.,arefactorsthataffect the brain blood flow and result in intracranial pressure changes. In theseries of patients presented, none of the alterationsmentionedabovemanifested.
Basedonclinicalorneuropathologicalgrounds,thereare insufficient data to attribute this syndrome to an incre-mentinbraintissuemass.Signsofmentaldysfunctionare commonly found in other neurological stateswhere there is diffuse cerebral edema, such as alcoholicor hyperten-siveencephalopathy.Infact,ifthediffusecerebraledema existed in BIH, its severity would not be enough to raise intracranialpressureand atthe sametimepreserve men-tal state. Despite this, cerebral edema cannot be totally excluded asthe physiopathological base of this problem. At the moment of surgery, 9 patients of this series pre-sented bulging of the brain after dural incision. One of them wasa childwithlateral venoussinus occlusion.Due to the lack of retention of CO2 during anesthesia, this
finding suggested the presence of ‘‘cerebral swelling’’. The pneumoencephalographic finding of small ventricles in some of these patients suggested this alteration as well.
With the exception of the rare cases of autopsies in patientswithintracranialvenoussinusesthrombosisandotic infection, where the brain was found to be normal, the mainsourceofpathologicalmaterialinBIHpatientscomes frombrainbiopsies.Changesof saidspecimenshavebeen describedas‘‘consistentwithcerebraledemaaffectinggray matteraswellaswhite,includingintracellularand intersti-calzones’’.However,thesefindingshavebeenconsidered contrived.Inthisseries,cerebralbiopsieswereperformed in5patients,noneofwhomdisplayedcerebralbulging dur-ingsurgeryandgrayandwhitematter werefoundtohave normalcharacteristicsintheroutinehistologicalexam;the brainoftheobesewomanwhodiedasaresultoftechnical operativedifficultieswasnormal,exceptfortheiatrogenic hemorrhageoftheposteriorfossa,andthesmallpituitary acidophiltumor.Thereisnoreportofelectronicmicroscopic studiesorbiochemicaldeterminationsinthestudiedtissue indifferentreportsofmedicalliterature.
Unfortunately,therearenoreliablemethodswhichcan measureCSFvolumeinhumanbeingsinapreciseway; how-ever,thefindingsinthepresentseriesfavorthehypothesis that,at leastinsomeBIHpatients, therewasanincrease in CSF. In 46 patients, at the timeof ventriculography or decompressive surgery, it was noted that there was an ‘‘enlargement’’ofthesubarachnoidspacewithCSFas ten-sion.Byaffectingthearachnoid,theliquidflowedtowards theoutsideandthenormalbrainor‘‘wetbrain’’seemedto reintegratewithinthelimitsofthecranialcavity.Thisrare findingof adilatedsubarachnoid space,witha normalor ‘‘small’’ventricularsystem, hasbeen foundrepeatedlyin differentreportsintheliterature.Foleyhasreferredtothis findingas contrivedand it has been named a part of the general edematousprocess bySahs and Joynt. Symmonds considersittobetheresultofanalterationinthefunction ofarachnoidgranulations,andasapossiblemanifestationof somephysiologicaldefectintheabsorptionofCSF, accord-ingtoSilverstone. This apparent CSF‘‘enlargement’’was greater than normal. According to certain authors, such Foley,Sahs,SolisandSweet,ifthiswerecorrect,the ventri-cleswouldbebiggerthannormal,andsincesmallornormal ventricleshavebeenfoundinthissyndrome,thispossibility hasbeendiscarded.
Inthepresentseries,theAyalaindex,whichcanbe con-sideredagrossassessmentofCSFvolume,waselevatedin34 outof41patients.Thereismuchcriticismaboutthevalidity ofthisprocedure; despitethis,in absenceofamore reli-abletechniquetomeasuretheamountofCSF,anelevated Ayalaindexsuggeststhatthefluidvolumewasgreaterthan normal.The presence inmany patients oflow proteinsin CSF,aswellasthosecasesreportedinmedicalliterature, wouldhavetosustainthisideaofanincreaseofCSFvolume, consideringthereisadilutioninitslevelofproteins.
ThedegreeofCSFformationhasbeencalculatedbased ontwodifferent techniques,in 15 cc. and450 cc. aday. Therehasn’tbeenanestimationofCSFformationin patho-logicalstates.Sweetet.al.reportedthattheconcentration of Na 24 in the ventricles of BIH patients was between 61 and88% of theplasmatic levelsan hour. These results were comparable to those obtained in a normal control. However,duetothefactthatitisnotpossibletodirectly relate the degree of sodiumentrance tothe presence of intracranialhypertension,itisnotpossibletomakean inter-pretationofthefluidexchangedynamic.Inthisreport,CSF and serum osmolarity were the same in 4 patients. This seemstoexcludethepossibilitythatthereisanincreasein CSFvolumeduetothedifferencesofosmoticpressure.The obstructionofthedrainageroutesshouldbeconsideredas apossiblecauseofCSFincrease.Inclinicalsituationswhere therearebasilararachnoiditis(i.e.tuberculousmeningitis) ora frankdilationofthe ventricles,impedingCSFflow,it ispossibletoobservedilationoftheventriclesinthe pneu-moencephalographicstudy andnotthenormalor‘‘small’’ ventricularsystemasseeninthissyndrome.Although,ifthe pointofobstruction werelocatedinthearachnoidvilli,it istobeacceptedthatinsteadofventriculardilation,there wouldbean increaseinCSFvolumethatwouldbeevenly distributedinthewholecraniospinalsubarachnoidspace,as wellasintheventricles,anditwouldbemanifestedonlyby adistendedsubarachnoidspace.WelchandFriedmanhave demonstratedthatsubarachnoidvillifunctionasvalvesor
aflowroute forCSFtowardsthevenoussinuses.However, thesestructureshavenotbeenstudiedinthissyndrome.
The pathogenesisof BIH inpatients withoticinfection is related to the obstruction of intracranial venous flow throughthe lateral venous sinus. In the present series,a compressionofthelateralvenoussinuswasobserved(with or without thrombosis) at the moment of mastoidectomy anditwasdemonstratedbycarotidarteriography.Themain pathwayforintracerebralvenousdrainageistheupper lon-gitudinalsinus,whichnormallydrains directlytowardsthe rightlateralsinus.Therightlateralsinusislargerthanthe left.This canexplainthehigherfrequencyofaffectionof therightsideinBIHsyndrome(11outof13cases).
In2patientswithobstructionoftheleftlateralsinus,it waspossible tosuggest thatthis wasthecrucialdrainage pathway,orthatthethrombusoriginatedwithinthelateral sinusandspreaduntilitoccludedthetorcularherophili,thus interferingwiththetotaldrainage.Asustainedelevationof intracranialvenouspressureproducesachronicriseinCSF pressure.Itispresumed thattheinadequacy ofantibiotic therapypriortothepatient’sadmission,theimmaturityof themiddleearandtheproximityofthelateralsinustothe underdevelopedmastoid aircells, arefactors resultingin thesinuspathologyobservedinBIHinchildren.The prepon-deranceofmaleoverfemaleremainsunexplained(12:1).
Sinusthrombosismaybeinvokedinpatientswithclosed cranial trauma, where the lesion of a venous sinus with majordrainage, or the extension of an incidental venous thrombosistowardsavitaldrainage zone,may have com-promisedthepressuresystem.Nevertheless,theabsenceof cranialfracturein all9patientsandthe negativityofthe carotidangiographicstudytendtodiscardthistheory.
In the syndrome associated with the administration of corticosteroids, pregnancy and the alteration of the metabolicor endocrinefunction,BIH pathogenesiscannot bebasedin venoussinus thrombosis,which is stressedby thenegativityoftheangiographicstudyin8patients,where noobstructionofthevenoussinuswasobservedinthe arte-riogram.
Inthe4childrenwhoreceivedtherapy with corticoste-roids shortly beforetheir admission, or in those whohad reducedthe medication dosage, intracranialhypertension couldhavebeenrelatedto‘‘relative’’adrenocortical insuf-ficiency.Therearenolabdata tobasethis hypothesis on andthesepatientsdidnotshowclinical manifestationsof thisproblem.Childrenwhoweretakenoffthe corticoste-roids after taking the medication for either a long or a shortperiodoftime,demonstratedstatesofrelativeadrenal insufficiencysubstantiatedbythedecreaseofexcretionof corticosteroids. In fact, therewas a report of 2 children withBIHandadrenalinsufficiency;thesechildrenhadbeen previouslyadministeredcorticosteroids.Theassociationof Addison’sdiseasewiththeincreaseofintracranialpressure in 2 patients has been reported. At the time of surgery thesepatientswereconsideredtohavecerebraledema.If thiswasin factcerebral edema, abiochemicalalteration could be expected in this tissue, similar to the salt and H2Oincreaseobservedintheedematoustissue(white
potas-sium and sodium exchange alterations, suggesting that, insuprarenal insufficiency, thereis an abnormality in the dynamicofintracranialfluidsandinthemechanismsofion exchange.However,thisdatatellsuslittleabouttheeffects of steroids in the brain. In view of the large number of patientsreceivingcorticosteroidtherapyandtheapparent rarityofBIHinsaidpatientsafterdiscontinuingthe medi-cation,onemust assumethatthereareadditionalfactors whichmust playan importantpart inthe pathogenesisof this syndrome. Even though it is thought that there is a certain hormone imbalance in women with alterations in their metabolic or endocrine functions, there is no con-vincinginformationwhichsuggestswhichhormonemaybe responsible for this syndrome. In fact, normal studies of adrenalandthyroidfunctions in10patientsstudiedinthe present series tend to eliminate the concept of hormone imbalance.Nowadays,consequently,withtheexceptionof patientswithmastoiditisandlateralsinusobstruction,BIH pathogenesisispurelyspeculative.
Treatment
EventhoughtheBIHdiagnosisisoftenestablishedonlyafter theencephalographyand/ortheangiographyhaveexcluded the possibility of a tumor lesion, the syndrome may be suspected in some patients, and diagnosed correctly and treateddefinitivelybasedonhistoryandclinicalfindings.
The otoscopic examination, mastoid radiographies and carotidarteriogram (venous phase)arethe most efficient elementsforthediagnosisofapatientwithobstructionof thelateralsinussecondarytooticinfection.Theangiogram helpstoexclude the presence of brain abscessor ventri-culardilation,whichcanbecausedbyasilentmassinthe mid-lineorposteriorfossa.Thespecificrecommended treat-ment is mastoidectomy, withthe extraction of infectious andnecroticmaterialwhichcoversthesigmoidandlateral venoussinuses,aswellasantibiotictherapy.Thereareno establishedcriteriafortheindicationofthrombectomy.CSF mustbeexamined,lookingforthepresenceofbloodorsigns of infection. In general, the use of anticoagulants is not desirable,duetothepossibilityofahemorrhagicinfarction whichaccompaniescerebralvenousthrombosis.Theuseof dehydrator agents(intravenous urea)is theoretically con-traindicatedinviewofthepresenceofathrombosedvenous system. The resultingdehydration will certainly facilitate theformationorspreadingofvenousandsinusthrombosis. InadditiontothedropinCSFpressurewithosmotic diuret-ics,administeredinparenteralform,itisatemporaleffect (lessthan24hours)anditmaybefollowedbya‘‘rebound’’ effect.Thecontinuoususeofsaidagentsinorderto main-tainalow CSFpressurewouldbedangerous for thebrain as well as for other organs. There are very few rational basesfortheuseofanyoraldehydratoragent(liquid glyc-erin).However,other dehydrator agents have been used, suchasManitolat20%,withbetterresults,widetolerance andpracticallywithoutthe‘‘rebound’’effect.
Theprecedentofadministrationofcorticosteroids, par-ticularly when the dosage of the medication has been reducedor discontinued,suggests that thesyndrome is a resultofadrenalinsufficiency,andthatthespecifictherapy ishormonereplacement.Eventhough2ofthe4patientsin
thisseriesweretreatedwithhydrocortisone,theneedofa substitutivehormonetherapymaybequestioned,inviewof theasymptomaticclinicalstateofthepatients(Intherest oftheirapparatusandsystems),thelackofconfirming lab-oratorydataandtheexperiencewiththeother 2patients whowerenotadministeredspecifictherapy.
Inthepast,inordertoestablishaBIHdiagnosis,the diag-nosticprocedureofchoicewasaventriculography.However, thereisacertainreluctancetopracticeventriculographyin thepresenceofanormalor‘‘small’’ventricularsystem.As analternative,onemaysuggestbilateralcarotid arteriogra-phyfollowedbyapneumoencephalography,ifthetestwith contrastdoesnotindicateventriculardilation.Inthe pre-sentedseries,thedangerofventriculographywasconfirmed in4patientswhodevelopedsuddenworseningofvisionor deteriorationofvitalsignsafterthisdiagnosticprocedure.
Inobesepatients,atherapeuticmeasuremaybea reduc-tionofbodyweight.Inonepatientofthisgroup,thistype of treatment would besupported by the factthat in her, intracranial hypertension signs and symptoms reappeared after she regained the lostweight. The prolonged use of oraldiureticsandtherestrictionofsaltdidnotoffer addi-tionalbenefitstothepatientstreatedwithadietaryregime. Cortisonewasadministeredtopatientswithmenstrual irreg-ularitiesandBIHbutthereasoningbehindthistreatmentis stillindoubt.
Othermeasureshavebeenutilizedinordertomaintaina normalintracranialpressure,suchassurgicaldecompression andrepeatedlumbarpuncturesasasupportivetreatment. Thethreatofalterationinvisualfunctionisgenerallywhat callsfor theneed toapplythesemeasures.Outof the23 patients treated with repeated lumbar punctures, it was noted thatin 5 of them, CSFpressure wasashigh in the second puncture as it was in the original puncture per-formed 24to48hoursbefore.In14patients CSFpressure remainedabove200mmofH2Oattheendoftherepeated
lumbar punctures (up to 6 months later). Therefore the valueofseriallumbarpuncturesisnotclear.Inthisseries,23 patientswithaccentuateddeficitofthevisualfunctionwere surgically decompressed(subtemporal decompression);an improvementwasnotedin13.Nevertheless,thefearthat a permanent visual defect would emerge in 34 patients whodidnothavevisualdifficultiescausedthemtoundergo subtemporal decompression. In patients without a major alterationinthevisualfunction,wheretheefficacyofboth therapeuticformswasabletobeevaluated,therewasn’ta significantdifferenceinthe‘‘degreeofhealing’’amongthe 31 patientssurgicallytreated andthe 43patients treated with repeated lumbar punctures or simply managed with a close observation. Subtemporal decompression is not a totallyinnocuousprocedure,whichisprovenwiththeonset ofpost-operativefocalseizuresin5patientsandtransitory otorrhoeainanother.
Theinadequacy of bothsupportive treatmentsis made clearinthisseries,inwhich6surgicallytreatedpatientsand 6treatedwithrepeatedlumbarpunctureswerereadmitted between2weeksand7yearsaftertheirhospitaldischarge duetothereappearanceofintracranialhypertensionsigns andsymptoms.
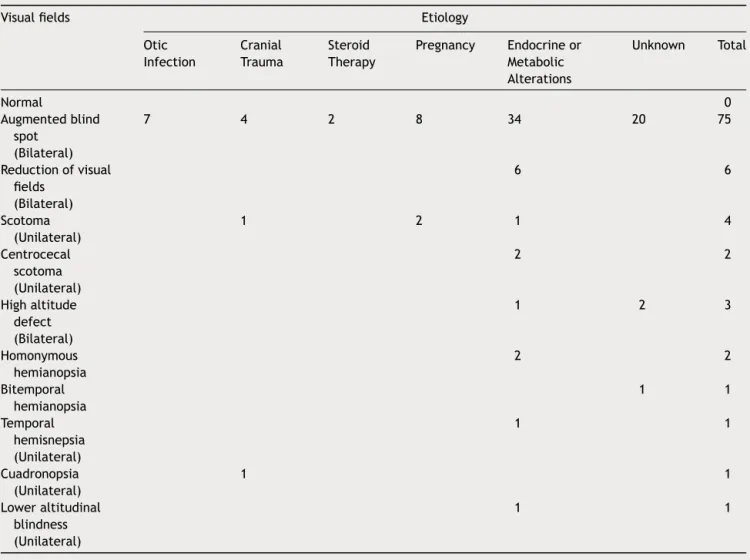
Table2 Findingsinvisualfieldsin80patientswithbenignintracranialhypertension.
Visualfields Etiology
Otic Infection
Cranial Trauma
Steroid Therapy
Pregnancy Endocrineor Metabolic Alterations
Unknown Total
Normal 0
Augmentedblind spot
(Bilateral)
7 4 2 8 34 20 75
Reductionofvisual fields
(Bilateral)
6 6
Scotoma (Unilateral)
1 2 1 4
Centrocecal scotoma (Unilateral)
2 2
Highaltitude defect (Bilateral)
1 2 3
Homonymous hemianopsia
2 2
Bitemporal hemianopsia
1 1
Temporal hemisnepsia (Unilateral)
1 1
Cuadronopsia (Unilateral)
1 1
Loweraltitudinal blindness (Unilateral)
1 1
aself-limitedsyndrome,andinabsenceofaspecific etiol-ogy,theremaynotbetheneedforsurgicaldecompression or repeated lumbar punctures. Certainly, in cases where papilledemaand otherintracranialhypertension signsand symptoms improve or are reduced after diagnostic tests, they may require just an observation period. Neverthe-less,theprogressionofthesefindingsinotherpatientsmay requirea morevigoroustreatment in theformof decom-pression or serial lumbar punctures. Although a frequent and repeatedexam of thevisual function may serveas a usefulguidetoassesstheneedforthisformoftreatment,a sudden decline in the visual function may be incorrigible by surgical decompression or lumbar punctures. The ele-vation ofCSFpressuremayalsoindicatetheneed for the institutionofamoredirecttreatment.ButanabnormalCSF pressure(above200mmofH2O)mayexistmonthsafterthe
patientleavesthehospital,when he/sheisasymptomatic and the papilledema has disappeared. The nature of the phenomenonisunexplained(Tables2---5).
Summary
Theclinicalcourseof102patientswithbenignintracranial hypertensionhasbeenrevised.Underthebasesofcommon
eventsoftheoutbreakofphysicalfindings,thesepatients maybedistributedinto6differentcategories:a)Otic infec-tion(13),b)Lightclosedheadtrauma(9),c)Corticosteroids therapy (4), d) Pregnancy (8), e) Probable metabolic or endocrinal alterations (39), f) A miscellaneous group not relatedtotheothergroups(29).Theetiologicalsignificance ofeachgroupisdiscussed.
Withtheexceptionofchildrenwithoticinfection,where thecauseof thesyndromeseemstobetheobstructionof thelateralvenoussinus,thepathogenesisintherestofthe groupsremainsobscure.Bothaspects,theexposedbrainand thesubarachnoidspaceduringsurgery,offeracluetowards thenatureofthesyndrome.Duringsurgery,thebulgingof thecerebralcortexwasobservedin9patients.Thissuggests cerebraledema,andthepresenceofnormalor small ven-tricleswouldbecompatiblewiththispossibility.However, we were able to observe a distention of the subarach-noidspace in46 patients. This, in additiontothe finding of a rise of persistent elevation of the Ayala index in 34 patients,wouldsupportthehypothesisofanincreasedCSF volume.
Table3 Correctedvisualacuityin80patientswithbenignintracranialhypertension.
Visualacuity Etiology
Otitis Cranial Trauma
Steroid Therapy
Pregnancy Endocrineor Metabolic Alterations
Unrelated Total
Normal 7 3 1 6 28 15 60
Uniocularacuity lessthan20/70
2 2 4
Binocularacuity lessthan20/70
1 1 4 5 11
‘‘Finger-counting orlight’’ UniocularVision
1 1 2
‘‘Finger-counting orlight’’ BinocularVision
1 1 2
Uniocular blindness
0
Binocular blindness
1 1
hydrocortisoneforthechildadmittedafterhavingreceived corticosteroidtherapy,subtemporaldecompressionand/or repeatedlumbarpuncturesaretheutilizedmethods.In gen-eral, all these forms of therapy have been found to be inadequate.
Itis concludedthatinmanycases,BIHisaself-limited syndromeand,inabsenceofaspecificetiology,theuseof aggressive therapy may not be necessary. Therefore, the managementofeachpatientinparticularoughttobe indi-vidualized.
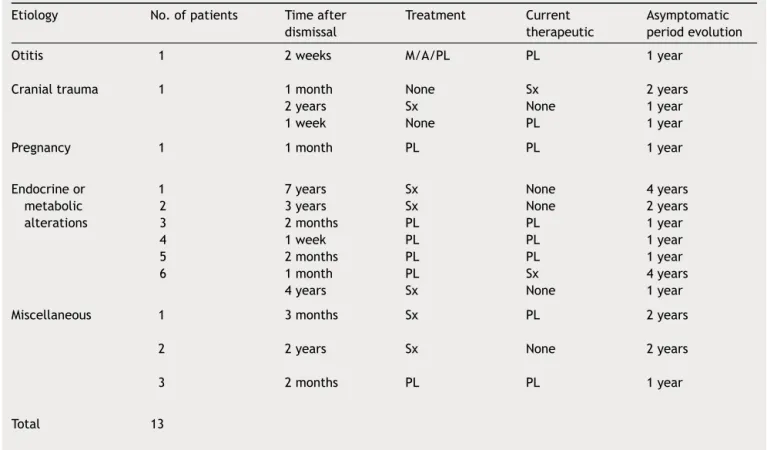
Table4 Evolutionof13of102patientsreadmittedwithbenignintracranialhypertension.
Etiology No.ofpatients Timeafter dismissal
Treatment Current therapeutic
Asymptomatic periodevolution
Otitis 1 2weeks M/A/PL PL 1year
Cranialtrauma 1 1month
2years 1week
None Sx None
Sx None PL
2years 1year 1year
Pregnancy 1 1month PL PL 1year
Endocrineor metabolic alterations
1 2 3 4 5 6
7years 3years 2months 1week 2months 1month 4years
Sx Sx PL PL PL PL Sx
None None PL PL PL Sx None
4years 2years 1year 1year 1year 4years 1year
Miscellaneous 1 3months Sx PL 2years
2 2years Sx None 2years
3 2months PL PL 1year
Total 13
Benign
Intracranial
Hypertension
(Cerebral
Pseudo-tumor)
13
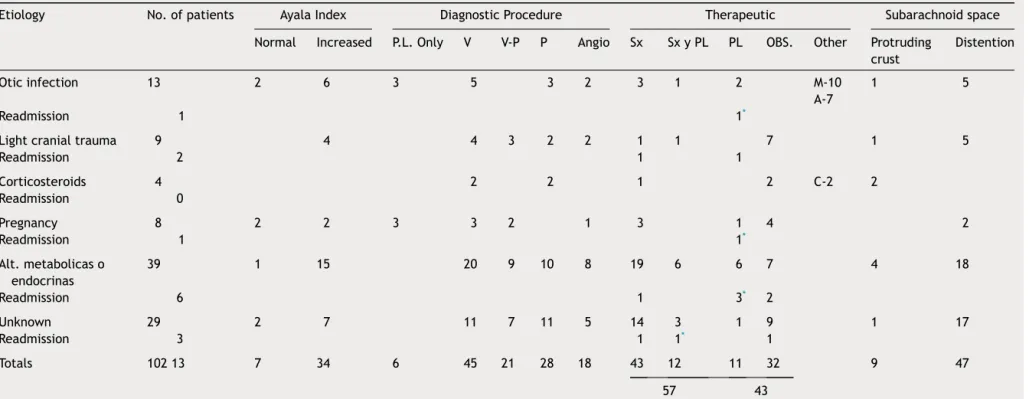
Table5 Diagnosticandtherapeuticmanagementof102patientswithbenignintracranialhypertension.
Etiology No.ofpatients AyalaIndex DiagnosticProcedure Therapeutic Subarachnoidspace
Normal Increased P.L.Only V V-P P Angio Sx SxyPL PL OBS. Other Protruding crust
Distention
Oticinfection 13 2 6 3 5 3 2 3 1 2 M-10
A-7
1 5
Readmission 1 1*
Lightcranialtrauma 9 4 4 3 2 2 1 1 7 1 5
Readmission 2 1 1
Corticosteroids 4 2 2 1 2 C-2 2
Readmission 0
Pregnancy 8 2 2 3 3 2 1 3 1 4 2
Readmission 1 1*
Alt.metabolicaso endocrinas
39 1 15 20 9 10 8 19 6 6 7 4 18
Readmission 6 1 3* 2
Unknown 29 2 7 11 7 11 5 14 3 1 9 1 17
Readmission 3 1 1* 1
Totals 10213 7 34 6 45 21 28 18 43 12 11 32 9 47
57 43
V=Ventriculography;V-P=Ventriculographyineffective,Pneumoencephalographyperformed;P=Pneumoencephalography;ANG=Carotidangiography;Sx=Subtemporalorsuboccipital decom-pression;Sx&PL=Seriallumbarpuncturesafterdecompression;PL=Seriallumbarpunctures;M=Mastoidectomy;A=Antibiotics;C=Hydrocortisone;OBS=Clinicalobservation(includinga reduceddietwith27obesepatients).
CORTEZAPROMINENTE=Brainprotrudedthroughincisioninhardandaranoides. Distention=Thesubarachnoidspaceappearsdistended.
References
1.FoleyJ.Benignformsofintracranialhypertension---‘‘Toxic’’ and‘‘Otitic’’hydrocephalus.Brain.1955;78:1---41.
3.AyalaG. Die Physiopathologieder Mechanikdesliquor cere-brospinalis and derRachidealquotient.Montasschr PsycliatU Neurol.1925;58:65---102.
4.Greer,M.:BenignintracranialhypertensioninobesewomenVI Neurology(Minneap)15:382.
7.BellerAJ. Benign post-traumatic intracranial hipertension. J NeurolNeurosurg&Psychiat.1964;27:149---52.
8.Greer M. Benign intracranial hypertension II Following corticosteroid therapy. Neurology (Minneap). 1963;13: 439---41.
9.GreerM.Benignintracranialhypertension.IVMenarche Neurol-ogy(Minneap).1964;14:569---83.
10.Walsh FB. Papilledema associated with increased intracra-nialpressure inAddison’s disease. ArchOphtalmology. 1952; 47(86).
11.Deranney JW, Shea JH. Allergic encephalopathy with papilledemaA.M.A.ArchNeurol&Psychiat.1952;68-791-793. 13.GreerM.BenignintracranialhypertensionVMenstrual
dysfunc-tion.Neurology(Mineap).1964;14:668---73.
14.GerberA,ReabAP,SobelAE.VitaminApoisoninginadults.Am JMed.1954;16:729---45.
15.Fremont Smith, F., Donley, M.E. and Thomas, G.W. Dilution ofbloodandcerebrospinalfluidinfever.J.Clin.Invest.6:9, 1928-9.
Further
reading
2.FordF.Diseasesofthenervoussystemininfancy,childhoodand adolescence.4re EdSpringfield,111,CharlesC.Thomas,Co; 1960.p.p889.
5.Paterson R, DePasquale N, Mann S. Pseudotumor cerebri. Medicine.1961;40:85---9.
6.GreerM.Benignintracranialhypertension.IMastoiditisand lat-eralsinusobstruction.Neurology(Minneap).1962;12:472---6. 12.GreerM.Benignintracranialhypertension.III-Pregnancy.
Neu-rology(Minneap).1963;13:670---2.
16.Gardner WJ, Spitler DK, Whitten C. Increased intracranial pressure by increased protein in the CSF. New Eng J Med. 1954;250:932---6.
17.Greer,M.:Benignintracranialhypertension.(pseudotunor cere-bri)inchildren.(Porpublicarse).
18.WoodburyDM,TimirasPS,VernadakisA.Influenceof adrenocor-ticalsteroideonbrainfunctionandmetabolism.In:Hormones, BrainFunctionandBehavior.NewYork:AcademicPress;1957. p.27---54.
19.Jefferson A. A Clinical correlation between encephalopathy and papilledemain Addison’s disease. JNeurol Neurosurg& Psvchiat.1956;19:21---7.
20.Dees SC, McKay HW Jr. Ocurrence of pseudotumor cerebri (benugnintracranialhypertension)duringtreatmentofchildren withasthmabyadrenalsteroids.Pediatrics.1959;23:1143---51. 21.KinalME,JaegerRM.Thrombophebitisofduralvenoussinuses