Multiple Sclerosis (MS) is a chronic autoimmune disease of the Central Nervous System (CNS) characterized by infl ammation, demyelination and axonal degeneration (Kornek & Lassmann 2004). It is the second cause of disability in young adults (Nieto, Sánchez, Barroso, Olivares, & Hernández, 2008). Typically, MS leads to disability because of cumulative motor, sensory and or visual defi cit. Between 45 and 65% of the patients develop variable cognitive dysfunction over the course of the disease, being generally more frequent and severe in late phases (6 - 10%) and coexisting with physical impairment (Halligan, Reznikoff, Friedman, & La Rocca, 1988). However, cognitive dysfunction can be a major complaint and the main cause of disability in the initial stages and, in contrast to motor or sensory defi cits, it does
not tend to improve (Calabrese et al., 2009; Staff, Lucchinetti, & Keegan, 2009). When cognitive deterioration in MS becomes the predominant symptom, it has been named ‘Cortical MS’ by some authors (Zarei, Chandran, Compston, & Hodges, 2003).
Although in MS there is no specifi c pattern of cognitive dysfunction, the functions most commonly impaired are speed of information processing (SIP), attention, memory, executive functions (EF) and visuospatial and visuoconstructive abilities (Arango-Lasprilla, DeLuca, & Chiaravalloti, 2007; Genova, Sumowski, Chiaravalloti, Voelbel, & DeLuca, 2009; Patti, 2009). The brief batteries designed for the routine study of cognitive dysfunction in MS basically include the assessment of these functions (Boringa et al., 2001; Duque et al., 2012). The presence of neuropsychological syndromes (NPS) (cognitive and behavioural disorders observed in cerebral disease with involvement of cortical areas: agnosia, aphasia, apraxia) has only been described in isolated cases of MS, largely without regulated neuropsychological evaluation. Anecdotal cases have been published referring to acute aphasia (Devere, Trotter, & Cross, 2000), alexia with agraphia (Day, Fisher, & Mastaglia, 1987), alexia without agraphia (Dogulu,
ISSN 0214 - 9915 CODEN PSOTEG Copyright © 2013 Psicothema www.psicothema.com
Neuropsychological syndromes in multiple sclerosis
Mª José Gil Moreno
1, Marta Cerezo García
2, Raluca Marasescu
2, Ana Pinel González
2, Laudino López Álvarez
3and Yolanda Aladro Benito
21 Hospital de Móstoles, 2 Hospital Universitario de Getafe and 3 Universidad de Oviedo
Abstract
Resumen
Background: Cognitive impairment in multiple sclerosis (MS) is common (45-65%).Defi cits occur in speed of information processing (SIP), memory, attention, executive functions (EF) and visuoconstruction.Involvement of cognitive functions like language and gnosis is rare and lesser known. Our aim is to describe the cognitive function and the clinical and radiological features of fi ve patients with MS and with neuropsychological syndromes (NPS). Method: Retrospective review of MS patients with NPS studied, using specifi c tests of SIP, memory, attention, EF, visuo-spatial abilities, praxis and language. Results: The sample included four women (3 relapsing-remitting MS/1 secondary progressive MS) and one man with primary progressive MS (aged between 30-55 years). Cognitive symptoms were the initial complaint in three cases. Three cases presented apperceptive agnosia and constructive apraxia, one case presented alexia with agraphia and the fi fth patient presented motor aphasia. Four patients suffered cognitive dysfunction considered typical of MS. Magnetic resonance imaging (MR) in all cases showed high lesion volumes in T1 and T2-weighted sequences. A good correlation was observed between cognitive defi cits and the location of the lesions in four patients. Conclusions: NPS may be the initial complaint in MS patients, often associated with other cognitive defi cits, and it shows a close relationship with lesion location.
Keywords: Multiple sclerosis, neuropsychological syndrome, cognitive impairment, visual gnosis, aphasia.
Síndromes neuropsicológicos en la esclerosis múltiple. Antecedentes: entre el 45-65% de los pacientes con esclerosis múltiple (EM) manifi estan défi cits cognitivos en velocidad de procesamiento de la información (VPI), atención, memoria, funciones ejecutivas (FE) y visuoconstrucción. La alteración del lenguaje y la gnosis visual es infrecuente y poco reconocida. El objetivo es la descripción cognitiva, clínica y radiológica de cinco pacientes con EM con síndromes neuropsicológicos (SNPS). Método: revisión retrospectiva de pacientes de EM con SNPS estudiados mediante test específi cos de atención, memoria, VPI, FE, visuoconstrucción, gnosis visual y lenguaje. Resultados: la muestra incluyó cuatro mujeres (3 EM remitente recurrente, 1 EM secundaria progresiva) y un varón con EM primaria progresiva (edades entre 30-55 años). Los défi cits cognitivos fueron el síntoma inicial en 3 casos. Tres presentan agnosia aperceptiva y apraxia constructiva, uno alexia con agrafi a y el quinto afasia motora. Cuatro asocian disfunción cognitiva “típica” de EM. En resonancia magnética observamos alto volumen lesional en secuencias potenciadas en T1 y T2 y correlación entre los défi cits cognitivos y la localización de las lesiones en 4 de ellos. Conclusiones: los SNPS pueden ser la queja inicial en la EM, con frecuencia se asocian a otros défi cits cognitivos y manifi estan una estrecha relación con la localización de la lesión.
Palabras clave: síndrome neuropsicológico, alteración cognitiva, gnosis visual, afasia, esclerosis múltiple.
Psicothema 2013, Vol. 25, No. 4, 452-460
doi: 10.7334/psicothema2012.308
Received: November 9, 2012 • Accepted: June 27, 2013 Corresponding author: Yolanda Aladro Benito Servicio de Neurología
Hospital Universitario de Getafe 28905 Getafe (Spain)
Kansu, & Karabudak, 1996; Mao-Draayer & Panitch, 2004), visual agnosia (Okuda et al., 1996) and patients with more than one severe cognitive symptom, with criteria for dementia (Staff et al., 2009; Stoquart-ElSankari, Périn, Lehmann, Gondry-Jouet, & Godefroy, 2010). When cognitive impairment is the initial and predominant symptom, it constitutes a diagnostic challenge (Calabrese, Filippi, & Gallo, 2010; Rinaldi, Calabrese, & Grossi, 2010).
The objective of this study is the cognitive assessment and the clinical and radiological description of fi ve patients with MS presenting with NPS, evaluated by means of specifi c cognitive tests.
Method
Participants and procedure
This study was conducted in the Multiple Sclerosis Unit, at the Getafe University Hospital. From a total of 164 patients with MS (McDonald 2005 diagnostic criteria) (Polman et al., 2005) and neuropsychological evaluation, fi ve were selected for presenting neuropsychological symptoms involving changes in cognitive processes such as language and visual gnosis.
An analysis of demographic data, course of the disease and degree of physical disability (Kurztke disability status scale, EDSS) (Kurtzke, 1983) was carried out at the moment of diagnosis of the NPS.
An estimate of the lesion volume was made by Magnetic resonance imaging (MR) axial T1- and T2-weighted sequences and coronal fl uid attenuated inversion recovery (FLAIR). A low lesion volume (LV) was defi ned by the presence of 9 or fewer small size lesions (≤ 1 cm of larger diameter), a moderate LV by the existence of more than 9 lesions, at least 2 being large (diameter between 1 and 2 cm) and high LV if there was at least one large confl uent plaque (larger than 2 cm in diameter). Cerebral atrophy was qualitatively measured by inspection of the width of sulci and of the third and the lateral ventricles in relation to age. Finally, we performed a second neuropsychological evaluation in some patients in order to estimate the progression or remission of the cognitive defi cits.
Instruments
From October 2004 to March 2012, an extensive routine neuropsychological evaluation was performed including the functions typically impaired in MS (IPS, memory, learning, attention and EF), language and visuospatial abilities. The degree of anxiety and depression was also measured with the Beck Depression Inventory (BDI) and Spielberger’s State-Trait Anxiety Inventory (STAI). Values lower than the normative values of each test were considered pathological.
Clinical cases
A summary of the clinical and radiological characteristics, as well as the results of the cognitive tests, is found in Tables 1-5.
Case number 1 is a 33-year-old woman. In 2001, she had the fi rst
MS symptom, consisting of motor impairment of the right hand. The second fl are occurred in 2006 with motor-sensory impairment; therefore, the patient was diagnosed of relapsing-remitting MS (RRMS). Examination revealed signs of pyramidal, sensory and
gait impairment (EDSS score: 3). The patient did not experience symptoms of cognitive deterioration at any time. However, a protocol neuropsychological evaluation in 2007 found a normal intelligence and low to moderate changes in IPS, attention, EF and visuoconstruction. Because diffi culties at reading and writing were observed during the evaluation, additional linguistic processing was examined using the PALPA battery (Spanish version EPLA: Valle & Cuetos, 1995). The patient presented adequate phonological processing in the differentiation of sounds, letters and words independently of the imageability, frequency of use or morphology. She repeated sentences well and exhibited a good level of picture naming. Signifi cant diffi culties were observed in reading and writing, and she showed signifi cant effects of imageability, frequency of use and infl ectional morphology. The patient also had diffi culties reading non-words, writing functional words and she committed errors depending on derivational morphology. These diffi culties resulted in mistakes in the orthographic input lexicon and in grapheme-phoneme conversion (see Table 1). Symptoms of fatigue, anxiety and depression were also present. Cranial MR showed multiple large demyelinating lesions, some confl uent in the deep white matter (WM) in both cerebral hemispheres, predominantly in the left parietal-occipital-temporal area, clear cortical atrophy and a thinning of the corpus callosum (Figure 1). At a new neuropsychological evaluation in 2009, a remission of her alexia-agraphia syndrome was observed.
Case number 3 is a 43-year-old woman with secondary progressive multiple sclerosis (SPMS) of 10 years of evolution and an EDSS score 5 by impairment of walking, associated with mild decrease of visual acuity (>20/30) and fatigue. She complained of spatial disorientation, often getting lost in places close to her home. The fi rst neuropsychological evaluation in April 2004 found
diffi culties in the visual perception of objects and space, and in the construction of fi gures under visual guidance. The patient had problems in integrating fi gures into a whole, in the mental rotation of fi gures and elements and also in using three-dimensionality. These defi cits were explained by apperceptive visual agnosia, spatial agnosia and moderate constructional apraxia and were not
Table 1
CASE 1: Clinical details and cognitive results
Sex
Level of education (years of schooling)
Age in the fi rst neuropsychological evaluation (NPSE). EDSS in the fi rst NPSE.
Disease duration in the fi rst NPSE (Years).
MRI:
T1 lesion volume •
T2 lesion volume • Cerebral atrophy • Female 11 33 3 6 High High Yes TESTS SCORES 2007 SCORES 2009 Normative values
WAIS-III (Wechsler Adult Intelligence Scale) Digit Symbol-Coding
Block Design Symbol Search Letter-number sequencing
WMS-III (Wechsler Memory Scale) Logical Memory I
Family Pictures I Logical Memory II Family Pictures II
Rey Osterrieth Figure (ROCF)
Type of the copy Accuracy of copy Time of copy Immediate recall condition
BNT (Boston Naming Test) Total Score
CTMT (Comprehensive Trail Making Test) Tests 1/2/3/4/5
Index
BADS (Behavioural Assess. of Disexecutive Syndrome) Temporal Judgement
Zoo Map
WCST (Wisconsin Card Sorting Test) Total % of errors
% Perseverative Responses Nº of categories completed Trials to complete 1st category Failure to maintain set Learning to Learn
PALPA (Psycholinguistic Assessment of Language) Reading
Letter discrimination W/NW
Visual lexical decision HIHF/HILF/LIHF/ LILF Visual lexical decision. fl ex./deriv./non-word. Reading HIHF/HILF/LIHF/ LILF Reading regular/Irregular. Non words reading 5 letters/6 letters Reading sentences
Writing
Writing length 5 letters/6 letters
Writing to dictation HIHF/HILF/LIHF/ LILF Writing to dictation Noun/Adjective/Verb/function Writing imageability. Nouns/functional W Writing to dictation Regular/ Derived/ Irregular Writing non-words 5 letters/6 letters
Max Score 7 4 5 7 Max Score 10 13 11 12 Percentile 75 60 75 70 Raw Score 58 Standard. S 28/29/24/19/27 23 Profi le
2 2 Percentile 90 94 >16 >16 >16 >16 Z score 0.63/-2.63 0/-9.2/-4.2/0.55 -2.8/0.33/7.9 0.23/0.23/-3.27/0.58 0.35/0.1 -1.38/-0.62 -1.91 Z score 0/0.3 -1.91/-2.1/-4.25/-0.35 -1.2/0.31/0.31/-3.4 -1.78/-3.71 -3.4/-3.9/-1.68 0.27/-1.72 Max Score 6 8 6 9 Max Score 13 16 13 19 Percentile 75 80 50 30 Raw Score 57 Standard. S 26/34/37/30/29 29 Profi le
2 4 Percentile 86 92 >16 >16 >16 >16 Z score 0.54/-0.73 0/0/0/0 -0.92/0.33/0.45 0.23/0.23/0.23/0.58 0.35/0.1 -0.33/-0.33 0 Z score 0/0.3 0.64/0.35/0.66/-0.35 -0.53/0.31/0.31/-0.35 -0.35/0 0/0.23/-0.36 0.27/-0.95 Max Score 10 10 10 10 Max Score 10 10 10 10 Percentile 50 50 50 50 Raw Score 54 Standard. S 50 50 Profi le
justifi ed by the degree of visual impairment (see Table 3). The patient also showed alterations in other cognitive functions: IPS, attention, EF and verbal and visual episodic memory. The cranial MR showed confl uent periventricular demyelinating lesions, and other multiple non-confl uent lesions in frontal and parietal and occipital areas, corpus callosum and also infratentorial, as well as signs of signifi cant axonal damage and subcortical and cortical atrophy. In a second neuropsychological evaluation in 2009, cognitive performance was similar, and no progression of visual agnosia was found. However, she showed a slight decrease in SPI and EF. On the other hand, the patient displayed a high level of fatigue, symptoms of mild depression and mild anxiety.
Case number 4 is a 44-year-old woman with a very active form of RRMS, both clinical and radiological. She suffered her fi rst episode of the disease in 2006, with visual problems that impeded her from moving into familiar places. In the following months, she experienced several relapses with sensory impairment and unstable gait. At a new neurological evaluation performed a year and a half later, cognitive impairment was observed together with pyramidal signs and mild cerebellar involvement, with an EDSS score of 3.5 (excluding cognitive impairment). In the neuropsychological evaluation, severe cognitive defi cits were found: apperceptive visual agnosia, spatial agnosia, constructional apraxia, ideomotor apraxia and a signifi cant alteration in coding and recovery of verbal episodic memory. She also exhibited dysfunctions in EF and naming (Table 4). A behavioural disorder was also observed, including infantilism and emotional liability. A mood disorder with marked symptoms of depression and anxiety was also present. The cranial MR showed multiple demyelinating lesions at periventricular and yuxtacortical level, with a relative predominance in the parietooccipital areas, and also an important number of lesions in the brain stem. There were an elevated number of black holes and several of the occipital lesions showed gadolinium enhancing. The patient was treated with different immunomodulating drugs from the beginning, but her cognitive dysfunction progressed incessantly to fully developed dementia. In 2011, after 5 years, the patient was in a state of absolute dependence, needing 24-hour care.
Case number 5 is a 57-year-old male patient with a history of hypertension and high levels of cholesterol. His relatives requested medical attention after observing progressive cognitive deterioration in the last 2 years, which impeded him from performing the required tasks at work. The patient, a waiter by profession, forgot the customers’ orders, confused spaces at home and at work, had expression diffi culties and was notably indifferent about his mistakes. The neurological exam showed only cognitive impairment (EDSS score 0, without considering cognitive impairment). The neuropsychological evaluation confi rmed visual impairment in the perception of shape and space (apperceptive visual agnosia) and in colour naming (colour anomie), while maintaining perception of colour, topographical spatial disorientation, visuoconstructional impairment, preserving gestalt and simplifi cation and ideomotor praxis for transitive gestures. The patient maintained verbal comprehension and the repetition of words but failed in the repetition of non-words. When dealing with spontaneous oral and verbal expression, there was a notable loss in naming abilities, construction of simple, grammatically incorrect sentences and hesitation. A decrease in the use of functional words and the presence of phonological and semantic paraphasia were also observed. Reading was considered adequate albeit slow and with some diffi culty depending on the length of the sentence and presence of non-words. Verbal expression was the most affected, with diffi culties with substitution, addition and omission, especially in longer and less frequent words. Spontaneous writing was characterized by grammatically incorrect sentences and a decrease in the use of functional words. These defi cits resulted in diffi culties in the phonological output lexicon, in acoustic-phonological conversion and in phoneme-grapheme conversion. Finally, the patient showed a low to moderate decrease in verbal episodic memory (coding), IPS, attention and EF (Table 5) as well as marked apathy. In another neuropsychological evaluation carried out 8 months later, mild progression of language disorder (anomie), semantic memory and free verbal long-term memory Table 2
CASE 2: Clinical details and cognitive results
Sex
Level of Education (years of schooling) Age in neuropsychological evaluation (NPSE). EDSS in NPSE.
Disease duration in the NPSE (years).
MRI:
T1 lesion volume •
T2 lesion volume •
Cerebral atrophy •
Female 12 30 3 1.8
Medium High
No
TESTS SCORE2010 NormativeValues
WAIS-III (Wechsler Adult Intelligence Scale) Digit Symbol-Coding
Block design Symbol Search Letter-Number sequencing
WMS-III (Wechsler Memory Scale) Logical Memory I
Family Pictures I Logical Memory II Family Pictures II
Rey Osterrieth Figure (ROCF)
Type of the copy Accuracy of copy Time of copy Immediate recall condition
BNT (Boston Naming Test) Total Score
CTMT (Comprehensive Trail Making Test) Tests 1/2/3/4/5
Index
BADS (Behavioural Assess. of Disexecutive Syndrome)
Temporal Judgement Zoo Map
WCST (Wisconsin Card Sorting Test) Total % of errors
% Perseverative Responses Nº of categories completed Trials to complete 1st category Failure to maintain set Learning to Learn
PALPA (Psycholinguistic Assessment of Language processing in Aphasia)
Discrimination minimal pairs words Equal/ Different Auditory lexical decision HIHF/ HILF/LIHF/ LILF
Repetition: Length 3L/4L/5L/6L
Repetition: non-words 3L/4L/5L/6L
Max Score 5 10 7 8 Max Score
2 9 1 8 Percentile
75 90 50 50 Raw Score
55 Standard S 33/29/29/29/38
29 Profi le
1 2 Percentile
79 92 >16 >16 >16 >16 Z score
0.36/0.42
0/0/0.23/-0.35/-0.6 0.17/0.23/0.23/0
-3.27/-4.33/0.31/0.53
Max Score 10 10 10 10 Max Score
10 10 10 10 Percentile
50 50 50 50 Raw Score
54 Standard S
50 50 Profi le
2 2 Percentile
50 50 >16 >16 >16 >16 Z score
0 0
0
were all found. In the case history fi le collected from the family, the great effect of these diffi culties on this patient’s daily life activities could clearly be seen. The MR showed multiple lesions in the periventricular WM of both hemispheres and confl uent plaques in the parietal-temporal-occipital areas (Figures 3b and c). Two cerebrospinal fl uid samples examined in two different laboratories showed intrathecal IgG synthesis. Another MR performed one year later showed a new large left parietal yuxtacortical lesion.
Discussion
The patients we have described herein represent a particular clinical form of MS characterized by impairment in cognitive functions rarely affected in this disease, such as aphasia, alexia, agraphia and visual agnosia. Even though these cognitive processes are generally disturbed in cortical lesions, different pathological processes of the subcortical white matter can cause similar clinical syndromes (Damasio, 1992; Naeser et al., 1982).
Table 3
CASE 3: Clinical details and cognitive results
Sex
Level of education (years of schooling)
Age in the fi rst neuropsychological evaluation (NPSE). EDSS in the fi rst NPSE.
Disease duration in the fi rst NPSE (years).
MRI:
T1 lesion volume •
T2 lesion volume • Cerebral Atrophy • Female 8 43 5 10 Moderate High Yes TESTS Scores 2004 Scores 2009 Normative values
WAIS-III (Wechsler Adult Intelligence Scale) Digit Symbol-Coding
Block design Digit Span Symbol search Letter-Number sequencing
WMS-III (Wechsler Memory Scale) Logical Memory I
Family Pictures I Logical Memory II Family Pictures II Spatial Span
Rey Osterrieth Figure (ROCF)
Type of the copy Accuracy of copy Time of copy
Immediate recall condition
BNT (Boston Naming Test) Total score
CTMT (Comprehensive Trail Making Test) Tests 1/2/3/4/5
Index
BADS (Behavioural Assess. of Disexecutive Syndrome) Temporal Judgement
Zoo Map
Verbal Fluency
Phonemic Fluency (FAS)
Semantic Fluency (animals, fruit, supermarket)
WCST (Wisconsin Card Sorting Test) % total errors
% Perseverative Responses Nº of categories completed Failure to maintain set Learning to Learn
VOSP (Visual Object and Space Perception Battery) Screening Test Incomplete Letters Silhouettes Object decision Progressive Silhouettes Dot counting Position Discrimination Number location Cube analysis Scaled Score 2 5 8 5 10 Scaled Score 7 6 5 7 5 Percentile 50 1 10 10 Raw Score 50 Standard S 18/18/18/18/18 18 Profi le
3 1 Raw - Average
6 12 Percentile 5 7 6 >16 >16 Raw Score 20 16 12 14 14 6 20 6 4 Scaled Score 2 5 7 4 8 Scaled Score 7 6 5 7 5 Percentile 50 1 25 1 Raw Score 52 Standard S 18/18/18/18/18 18 Profi le
3 1 Raw - Average
6 12 Percentile 3 1 2 6 -Raw Score 19 11 17 10 13 1 13 7 6 Scaled Score 10 10 10 10 10 Scaled Score 10 10 10 10 10 Percentile 50 50 50 50 Raw Score 54 Standard S 50 50 Profi le
2 2 Raw - Average
Our first reported patient developed mild alexia with phonological agraphia in the context of a disease relapse, coincident with lesions in the left parietal and occipital areas, all evolving to complete remission at a later date. This defi cit presented only a very mild repercussion in her daily life and social and occupational activities. In the second case, motor aphasia due to a large lesion in the WM of the left hemisphere was the fi rst sign of disease, and it was not associated with any change in other cognitive functions and it also subsequently remitted. In this patient, the neuropsychological exam showed a large discrepancy between verbal and visual performance, not in accordance with spontaneous expression observed in normal conversation. This incongruence and the slight reduction in performance on SPI and attentive tasks can be explained by the elevated degree of anticipatory anxiety observed during the evaluation, as other authors have already observed (Nieto et al., 2008; Schulz, Kopp, Kunkel, & Faiss, 2006). The neuropsychological exam of the last three patients showed apperceptive agnosia and constructive apraxia in correspondence with bilateral lesions in the parietal and occipital areas. The last patient also showed alterations in linguistic processing. All but one of the cases (Case 2) exhibited cognitive impairment typical of MS, with some defi cit in the encoding of verbal memory, SPI, attention and EF, similar to those described
by other authors (Day et al., 1987; Devere et al., 2000; Okuda et al., 1996). We would like to highlight in three of our cases the good correlation encountered between apperceptive visual agnosia and the lesions observed in the parietal and occipital WM areas. Also remarkable is the recovery of language alterations observed in two of the patients.
NPS may be the initial form of presentation of MS (cases 2, 4 and 5) (Devere et al., 2000; Dogulu et al., 1996; Mao-Draayer & Panitch, 2004) or, more frequently, they may appear in the course of the disease in association with physical disability involving other functional systems (Cases 1 and 3) (Day et al., 1987; Okuda et al., 1996). When they constitute the only symptom and occur progressively, as in our Case no 5, it can be diffi cult to establish a diagnosis of MS (Stoquart-ElSankari et al., 2010); in this setting, the presence of intrathecal synthesis of immunoglobulins may be of great help. A rapid progression of cognitive dysfunction along with severe functional deterioration and dementia over a short lapse of time has been described in some other sporadic cases, similar to our Patient 4 (Staff et al., 2009; Stoquart-ElSankar et al., 2010). Some patients with cognitive impairment also display changes in the emotional sphere, mostly euphoria, emotional instability, apathy and/or symptoms of depression, also observed in our patients (Zarei et al., 2003; Zarei, 2006).
The prevalence of NPS in MS is unknown. Possible explanations are the lack of studies focused on these specifi c cognitive defi cits, and the fact that routine tests used in clinical practice only contemplate patterns of cognitive impairment typical of MS (Boringa et al., 2001; Duque et al., 2012). In addition, the tests may be administered by non-specialized personnel not skilled enough as to detect other possible defi cits which could deserve a more specifi c investigation. In spite of this, their prevalence is presumably low, as these cognitive defi cits demand specialized care because of the serious functional disability that they usually generate. In fact, the presence of aphasia only represented 0.8% of the 2700 MS patients tested by Larner and Lecky (2007). In spite of this probably low prevalence, it is important to consider cognitive deterioration as a main symptom of MS, even in cases where other neurological disorders are minor, given their potential repercussion on socio-occupational activities.
The substrate of cognitive impairment of MS, and in these particular NPS, is possibly brain atrophy. It may be that in the neuropsychological disorders involving typically cortical areas (aphasia, agnosia, apraxia), the grey matter (GM) atrophy is more relevant than WM atrophy. For decades, we have known that around 20% of the lesions in MS are found in the GM (Brownell & Hughes, 1962), and its clinical relevance and its important contribution to cognitive symptomatology are well recognized. Three types of lesions are found in the cerebral cortex, namely cortical-subcortical lesions involving the white and grey matter, small perivascular demyelinating intracortical lesions, and extensive subpial demyelination bands that cover several gyri and three or four layers (Rudick & Trapp, 2009). Given the strong correlation between cognitive deterioration and cortical atrophy, it is highly probable that a large part of cognitive symptoms of MS was the result of progressive damage to the GM rather than a consequence of WM atrophy (Amato et al., 2004; Benedict et al., 2006).
Cognitive impairment in MS may lead to severe and permanent disability (Wynia, Middel, van Dijk, De Keyser, & Reijneveld, Table 4
CASE 4: Clinical details and cognitive results
Sex
Level of education (years of schooling) Age in neuropsychological evaluation (NPSE). EDSS in NPSE
Disease duration in NPSE (years).
MRI:
T1 lesion volume •
T2 lesion volume •
Cerebral atrophy •
Female 8 44 3.5 1.5
High High Yes
TESTS Score
2008
Normative values
WAIS-III (Wechsler Adult Intelligence Scale) Picture completion
Vocabulary Similarities Block Design Digit Span
WMS-III (Wechsler Memory Scale) Logical Memory I
Logical Memory II Mental control
Information and Orientation
Verbal fl uency
Phonemic fl uency (FAS)
Semantic fl uency (animals, fruit, supermarket)
VOSP (Visual Object and Space Perception Battery)
Screening Test Incomplete Letters Silhouettes Object decision Progressive Silhouettes Dot counting Position Discrimination Number location Cube analysis
Scaled Score 1 9 6 1 5 Scaled Score
3 1 3 Percentile 1 Raw -Average
10 14 Raw Score
18 0 2 5 20 4 11 0 1
Scaled Score 10 10 10 10 10 Scaled Score
10 10 10 Percentile 50 Raw -Average
12-13 17-18 Cut-off Score
2008) with signifi cant socio-occupational impact (Rao et al., 1991). It is therefore necessary to perform properly designed neuropsychological studies, conducted by specialized professionals, in order to diagnose and better characterize cognitive impairment in patients with MS.
Acknowledgements
This work has been partially financed with project
PSI2010/19348 of the Ministry of Science and Innovation and by Merc-Serono y Biogen Idec laboratories.
Table 5
CASE 5: Clinical details and cognitive results
Sex
Level of education (years of schooling)
Age in the fi rst neuropsychological evaluation (NPSE) EDSS in the fi rst NPSE
Disease duration in the fi rst NPSE (years)
MRI:
T1 lesion volume •
T2 lesion volume •
Cerebral atrophy •
Male 12 57 4 2.2
High High Yes
TESTS Score
March 2012
Score November 2012
Normative values
WAIS-III (Wechsler Adult Intelligence Scale) Block Design
WMS-III (Wechsler Memory Scale) Logical Memory I
Logical Memory II
Rey Osterrieth Figure (ROCF)
Type of the copy Accuracy of copy Time of copy Immediate recall condition
CTMT (Comprehensive Trail Making Test) TEST 1
TEST 5
Verbal Fluency
Phonemic fl uency (P) Semantic fl uency(animals)
VOSP (Visual Object and Space Perception Battery) Screening Test
Silhouettes Object Decision Number Location Cube Analysis
BNT (Boston Naming Test) Total Score
M@T (memory alteration test) Total Score
FAB (Frontal Assessment Battery) Total Score
Scaled Score 5 Scaled Score
6 5 Percentile
75 1 10 1 Standard
18 18 Raw Score
4 13 Raw Score
18 7 9 3 4 Raw Score
42 Raw Score
37 Raw Score
10
– – – – – – – – – – – – – – – – Raw Score
20 12 7 4 4 Raw Score
37 Raw Score
31 – –
Scaled Score 10 Scaled Score
10 10 Percentile
50 50 50 50 Standard
50 50 Raw Score
12-13 17-18 Cut-off Score
15 15 14 7 6 Raw Score
54 Cut-off Score
36 Cut-off Score
16
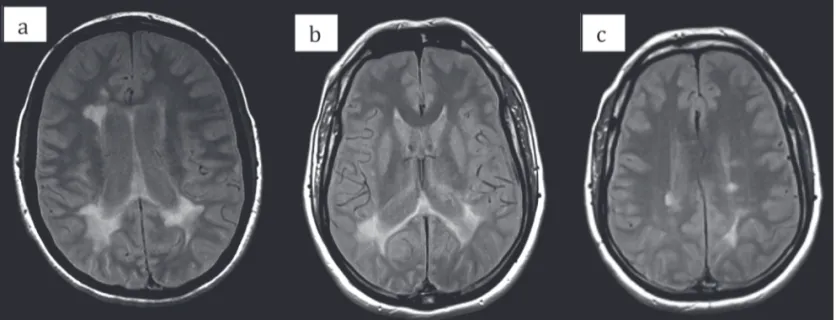
Figure 1. Brain MRI (axial sections), case nº 1: a) Multiple demyelinating
lesions, Some confl uent and an extensive lesion in the left parietal region in T2
weighted sequences; y b) marked cerebral atrophy in T1 weighted sequences
Amato, M.P., Bartolozzi, M.L., Zipoli, V., Portaccio, E., Mortilla, M., Guidi, L., et al. (2004). Neocortical volume decrease in relapsing-remitting MS patients with mild cognitive impairment. Neurology, 13, 89-93. Arango-Lasprilla, J.C., DeLuca, J., & Chiaravalloti, N. (2007). El perfi l
neuropsicológico en la esclerosis múltiple [Neuropsychological profi le of multiple sclerosis]. Psicothema, 19, 1-6.
Benedict, R.H., Bruce, J.M., Dwyer, M.G., Abdelrahman, N., Hussein, S., Weinstock-Guttman, B., et al. (2006). Neocortical atrophy, third ventricular width, and cognitive dysfunction in multiple sclerosis.
Archives of Neurology, 63, 1301-1306.
Boringa, J.B., Lazeron, R.H.C., Reuling, E.W., Adèr, H.J., Pfennings, L., Lindeboom, J., et al. (2001). The Brief Repeatable Battery of Neuropsychological Tests: Normative values allow application in multiple sclerosis clinical practice. Multiple Sclerosis, 7, 263-267. Brownell, B., & Hughes, J.T. (1962). The distribution of plaques in the
cerebrum in multiple sclerosis. Journal of Neurology, Neurosurgery &
Psychiatry, 25, 315-320.
Calabrese, M., Agosta, F., Rinaldi, F., Mattisi, I., Grossi, P., Favaretto, A., et al. (2009). Cortical lesions and atrophy associated with cognitive impairment in relapsing-remitting multiple sclerosis. Archives of
Neurology, 66, 1144-1150.
Calabrese, M., Filippi, M., & Gallo, P. (2010). Cortical lesions in multiple sclerosis. Nature Reviews Neurology, 6, 438-444.
Damasio, A.R. (1992). Aphasia. New England Journal of Medicine, 326, 531-539.
Day, T.J., Fisher, A.G., & Mastaglia, F.L. (1987). Alexia with agraphia in multiple sclerosis. Journal of the Neurological Sciences, 78, 343-348.
Devere, T., Trotter, J., & Cross, A. (2000). Acute aphasia in multiple sclerosis. Archives of Neurology, 57, 1207-1209.
Dogulu, C.F., Kansu, T., & Karabudak, R. (1996). Alexia without agraphia in multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry, 61, 528.
Duque, P., Ibáñez, J., del Barco, A., Sepulcre, J., de Ramón, E., Fernández-Fernández, O., et al. [Normalisation and validation of the Brief Neuropsychological Battery as the reference neuropsychological test in multiple sclerosis]. Revista de Neurología, 54, 263-270.
Genova, H.M., Sumowski, J.F., Chiaravalloti, N., Voelbel, G.T., & DeLuca, J. (2009). Cognition in multiple sclerosis: A review of neuropsychological and fMRI research. Frontiers in Bioscience, 14, 1730-1744.
Halligan, F.R., Reznikoff, M., Friedman, H.P., & La Rocca, N.G. (1988). Cognitive dysfunction and change in multiple sclerosis. Journal of
Clinical Psychology, 44, 540-548.
Kornek, B., & Lassmann, H. (2004). Neuropathology of multiple sclerosis-new concepts. Brain Research Bulletin, 61, 321-326.
Kurtzke, J.F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology, 33, 1444-1452. Larner, A.J., & Lecky, B.R. (2007). Acute Aphasia in MS Revisited. The
International MS Journal, 14,76-77.
Mao-Draayer,Y., & Panitch H. (2004). Alexia without agraphia in multiple sclerosis: Case report with magnetic resonance imaging localization.
Multiple Sclerosis, 10, 705-707.
Naeser, M.A., Alexander, M.P., Helm-Estabrooks, N., Levine, H.L., Laughlin, S.A., & Geschwind, N. (1982). Aphasia with predominantly subcortical lesion sites: Description of three capsular/putaminal aphasia syndromes. Archives of Neurology,39, 2-14.
Nieto, A., Sánchez, M.P., Barroso, J., Olivares, T., & Hernández, M.A. (2008). Alteraciones cognitivas en etapas iniciales de la esclerosis múltiple y su relación con el estado de ánimo, variables demográfi cas y clínicas [Cognitive impairment in the early phase of multiple sclerosis and its relationship with mood, demographic and clinical variables].
Psicothema, 20, 583-588.
Okuda, B., Tanaka, H., Tachibana, H., Iwamoto, Y., Takeda M., Kawabata, K., et al. (1996). Visual form agnosia in multiple sclerosis. Acta
Neurologica Scandinavica, 94, 38-44.
Patti, F. (2009). Cognitive impairment in multiple sclerosis. Multiple
Sclerosis, 15, 2-8.
Polman, C.H., Reingold, S.C., Edan, G., Filippi, M., Hartung, H.P., Kappos, L., et al. (2005). Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Annals of Neurology, 58, 840-846.
Rao, S.M., Leo, G.J., Ellington, L., Naurertz, T., Bernardin, I., & Unverzagt, F. (1991). Cognitive dysfunction in multiple sclerosis. Impact of employment and social functioning. Neurology, 412, 692-696. Rinaldi, F., Calabrese, M., & Grossi P. (2010). Cortical lesions and cognitive
impairment in multiple sclerosis. Neurological Sciences, 31, 235-237. Rudick, R.A., & Trapp, B.D. (2009). Gray-matter injury in multiple
sclerosis. New England Journal of Medicine, 361, 1505-1506. Staff, N.P., Lucchinetti, C.F., & Keegan, M. (2009). Multiple sclerosis with
predominant severe cognitive impairment. Archives of Neurology, 66, 1139-1143.
Figure 3. Brain MRI (axial sections, PD): a) case nº 4: Multiple demyelinating lesions, with relative predominance in the parietal and occipital areas; b y
c) case nº 5: periventricular lesions y confl uent plaques, parietal-temporal-occipital areas
Stoquart-ElSankari, S., Périn, B., Lehmann, P., Gondry-Jouet, C., & Godefroy O. (2010). Cognitive forms of multiple sclerosis: Report of a dementia case. Clinical Neurology and Neurosurgery, 112, 258-260. Schulz, D., Kopp, B., Kunkel, A., & Faiss, J.H. (2006). Cognition in the
early stage of multiple sclerosis. Journal of Neurology, 243, 1002-1010.
Valle, F., & Cuetos, F. (1995). EPLA: Evaluación del Procesamiento Lingüístico en la Afasia. Hove, UK, Lawrence Erlbaum Associates.
Wynia, K., Middel, B., van Dijk J.P., De Keyser J.H., & Reijneveld S.A. (2008). The impact of disabilities on quality of life in people with multiple sclerosis. Multiple Sclerosis, 14, 972-980.
Zarei, M., Chandran, S., Compston, A., & Hodges, J. (2003). Cognitive presentation of multiple sclerosis: Evidence for a cortical variant.
Journal of Neurology, Neurosurgery & Psychiatry, 74, 872-877.
Zarei, M. (2006). Clinical characteristics of cortical multiple sclerosis.